4
Preliminary findings from the National Youth Cultures of Eating Study – gender, social class and ethnic differences in childhood obesity
Introduction
Childhood obesity prevention has rapidly become one of the most controversial topics in current community, clinical and school health education debates. There is much talk of a global ‘epidemic’ of obesity in the academic literature (World Health Organization, 2003) as well as in the popular media. Some exclaim that the so-called ‘epidemic’ of childhood obesity will be ‘modernity’s scourge’ (Waters & Baur, 2003) and may reverse the observed improvements in life expectancy trends (Olshansky, Passaro & Hershow, 2005) whilst others more cautiously argue that current social comment about obesity is based on moral issues rather than true health risk (Campos, Saguy, Ernsberger, Oliver, & Gaesser, 2006; Gard & Wright, 2005; Rich & Evans, 2005). Others observe that children and adults can be both ‘fat and fit’ (Blair, 2005; Telford, 2007) and that the health risks of fatness may be largely over-ridden by physical activity. An important message for health professionals, school educators and social workers is to ‘first, do no harm’ when working towards obesity prevention among children (Ikeda, Crawford, & Woodward-Lopez, 2006; O’Dea, 2004). This is a particularly salient message for those working among different ethnic and cultural groups in the community.
Among the hundreds of published articles about childhood obesity there is a marked paucity of comment from the children themselves, and very little input invited from their parents (O’Dea, 2005). In one of the few studies of the socio-cultural contexts within which young people become fat and lay conceptualisations of fatness, Wills and her colleagues (2006) 80interviewed obese and overweight teenagers from socially disadvantaged areas in Scotland. In this study, the researchers found that these young people of low socioeconomic status (SES) had a high degree of body acceptance and rarely mentioned any health-related consequences of their fatness (Wills, Backett-Milburn, Gregory, & Lawton, 2006). Of weight-related importance to these young people, were fashion related issues and being physically ‘slowed down’.
Similarly, in successive studies of Australian adolescents over the past 15 years, I have observed social class differences in the prevalence of overweight and obesity as well as varying perceptions of the students’ weight and body image. In my earliest study of mid-adolescent girls from disadvantaged and non-disadvantaged backgrounds in 1991 (O’Dea, 1994) I found that the non-disadvantaged girls were significantly more likely to eat breakfast, dinner and an evening snack; take vitamin supplements and have better nutrition knowledge. The girls from disadvantaged backgrounds were nearly twice as likely to be obese or overweight (33% versus 19%), yet the desire to lose weight was present in nearly half (42%) of all the girls, irrespective of their SES. A later study was designed to further examine and clarify the SES, weight status and body image of 1134 children and adolescents in early 2000 (O’Dea & Caputi, 2001) and results reinforced the earlier findings that children of low SES were more likely to be overweight, obese and skipping breakfast. An illuminating finding of this study was that there was less body image concern and greater body esteem and physical self esteem among overweight boys and girls of low SES in comparison to their overweight middle or high SES peers. It appeared that these children and adolescents were clearly overweight, but it did not seem to bother them. A later study conducted nationally, confirmed the social class differences in overweight and obesity among nearly 5000 students from 38 randomly selected schools from every state and territory of Australia (O’Dea, 2003).
An obvious research question to evolve from these studies was whether the observed trends in obesity and SES were mainly related to SES via income, parental education or social disadvantage or whether there were other socio-cultural influences involved. One influence that was likely to be relevant was ethnicity or cultural background, as these factors had been identified among children in the USA (Kumanyika, 1993). Hence, the main aim of the current study was to examine the intersections of class, 81gender, age, and ethnicity as major factors affecting obesity, body image, food consumption and its meanings.
The importance of identifying cultural and ethnic issues in the management and prevention of weight-related disease has been recognised by several authors and is well illustrated in a recent study of Pakistani and Indian patients with Type 2 diabetes, conducted by Lawton and her colleagues (2006) in the UK. This study found that issues of social role, familial duties, perceived family cohesion and other issues related to the social roles of men and women in South Asian communities in the UK, were much more highly valued than self care (Lawton, Ahmad, Hanna, Douglas, & Hallowell, 2006). The authors of this study state that, ‘Education may play a role in physical activity promotion; however, health promoters may need to work with, rather than against, cultural norms and individual perceptions’ (Lawton et al., p. 52).
This article aims to explore the associations between obesity, weight perceptions and gender, ethnicity, culture and social class in a large national study of Australian schoolchildren. The paper also explores the most appropriate and effective approaches for educators, social workers and community health promoters when planning weight-related programs for children and adolescents.
Defining and Measuring Overweight and Obesity
In any discussion of weight, it is important to first understand the definitions, meanings and limitations of the measurement instruments. The strict definition of ‘obesity’ refers to ‘over fatness’ and is normally defined using some sort of measure of percent body fat such as skin fold thickness standards. Because of the costly, time consuming and invasive nature of these measures, most researchers undertaking large population studies of ‘obesity’ are necessarily required to use a proxy for obesity and overweight as defined by a measure of weight-for-height, the Body Mass Index [BMI] a measure of weight in kilograms divided by the square of height in metres. Many studies, including the current one, employ a general ‘international childhood BMI standard’ which has been developed by Cole, Bellizzi and Flegal (2000). The international standard creates a statistical distribution of BMI by extrapolating the childhood BMI distribution to track childhood and adolescent BMI equivalents to adult BMI 82cut off points of overweight (Adult BMI of 25 or more to 29.9) or obese (Adult BMI of 30 or more). Hence, the current international definition of childhood overweight and obesity is essentially a statistical definition of weight-for-height and gender and not body fatness per se. BMI is a screening tool, useful for making surveillance observations, but it is not a diagnostic tool and children with a BMI indicating obesity or overweight do not necessarily have any illness, clinical complications, or health risks associated with over fatness. More in-depth clinical assessment of individual children is required to ascertain their current health status and their future health risk (Flegal, Tabak, & Ogden, 2006) and the measures need to be monitored regularly over several years. Nevertheless, the current BMI-based definitions of overweight and obesity are generally useful working definitions that are valuable for public health surveillance, screening and community assessment.
Using various US and international BMI standards the prevalence of childhood overweight, obesity and increases in these over time have been measured in various countries to date. In the USA, the prevalence of childhood obesity has tripled since the 1960s with a low prevalence of about 3% in the 1960s to about 7–10% in the 1980s and 1990s (Flegal, Ogden, Wei, Kuczmarski & Johnson, 2001). The current prevalence in the USA is estimated at around 15% (Ogden, Carroll, & Curtin, 2006).
In the United Kingdom, analyses of three cross sectional studies of British children between 1974 and 1994 resulted in similar upward trends in childhood obesity prevalence to those observed in the USA (Chinn & Rona, 2001). Increasing prevalences have been observed in Australia (Magarey, Daniels, & Boulton, 2001), France (Huede, et al., 2003; Romon, Duhamel, Collinet, & Weill, 2005), Finland (Kautiainen, Rimpela, Vikat, & Virtanen, 2002), Portugal (Padez, Fernandes, Mourao, Moreira, & Rosado, 2004), Chile (Kain, Uauy, Vio, & Albala, 2002), Germany (Kalies, Lenz, & von Kries, 2002), Brazil, China and Russia (Wang, Monteiro, & Popkin, 2002).
Whilst the imminent risk of any illness in obese children is not considered common (Flegal et al., 2006), the risk for the development of insulin resistance and Type 2 diabetes is considered much more likely and serious with some cases of adolescents with these conditions already being diagnosed (Fagot-Campagna, 2000). Examples of such health risk for adolescents also includes an ethnic component with the vast majority of cases, whilst 83small in actual number, being diagnosed among very obese and very sedentary adolescents (Drake, Smith, Betts, Crowne & Shield, 2002), with a strong family history of Type 2 diabetes who often come from Indian, Pakistani (Ehtisham, Barrett, & Shaw, 2000) or African American or Native American backgrounds (American Diabetes Association, 2000). Similarly, about half of the 43 cases of Type 2 diabetes and related conditions identified over the 12 years from 1990 to 2002 in children and adolescents in Western Australia were found among Aboriginal children (McMahon et al., 2004) compared to those from other ethnic groups. A recent study of all medical register data on Type 2 diabetes in children and adolescents aged 7–18 years in the state of New South Wales (Craig, Femia, Broyda, Lloyd, & Howard, 2007) found 128 cases over the six years from 2001 to 2006 (about 21 cases each year). The authors reported that 90% of cases were overweight or obese. Aboriginal children were six times more likely to have Type 2 diabetes than their non indigenous peers and 75% had a family history of the disease. Whilst these ethnic and familial effects on Type 2 diabetes risk are not always apparent (Wiegand et al., 2004), they remain an important consideration.
Hence, any study of childhood obesity and its implications for child health and/or health education in our communities should currently include an assessment of gender, risk of actually developing any illness, and ethnicity.
Methods
Data in this study was collected as part of the National Youth Cultures of Eating Study which is a three-year, government funded study of health, weight, culture and eating among nearly 8000 schoolchildren drawn from every state and territory of Australia between August and November, 2006. The major aim of the study was to examine the intersections of class, gender, age and ethnicity as major factors affecting obesity, body image, food consumption and its meanings.
The questionnaire was constructed from previously validated instruments (Gracey, Stanley, Burke, Corti, & Beilin, 1996; O’Dea & Wilson, 2006) and completed by students in years 3–11 during regular class times under the supervision of trained research assistants. The questionnaire was developed for school years 3–4, 5–6 and 7–11 and measured demographic details of gender, age, ethnic background, weight perceptions (Do you think 84you are too thin (1), about right (2) or too fat (3)?); as well as other food- and nutrition-related questions, including those assessing eating habits, consumption of breakfast, nutritional quality of breakfast and beliefs about food and nutrition. Some open-ended questions were included in the instrument, but qualitative analysis of responses is not reported here. The details of the questionnaire have been described elsewhere (O’Dea & Wilson, 2006). Height and weight were measured by trained research assistants. Where literacy was an issue, the questionnaire was read aloud to the student by a trained research assistant.
Completed questionnaires were checked, edited, entered and cleaned to produce an SPSS data file. Descriptive and Chi square analyses were undertaken to provide details of the prevalence of obesity and overweight using the international standard with age in years taken to the 0.5 year cut-offs (Cole et al., 2000). Chi square analyses were used to examine group differences in prevalence of overweight and obesity between various ethnic and social class sub-groups of children and adolescents. BMI was analysed as the dependent variable using ANOVA performed separately for boys and girls with age as a covariate and ethnicity and SES as independent variables. All continuous data were checked to make sure they were normally distributed. Residuals were examined for normality, linearity and homoscedasticity and these assumptions were met.
The study was approved by the University of Sydney Human Ethics committee as well as each school principal and each of the Departments of Education in every state and territory of Australia. All students with informed parental consent were eligible to participate and each student’s verbal consent was obtained on the day of the study. No follow-up visits were undertaken.
Results
Participants
A total of 47 randomly selected primary and high schools were recruited from every state and territory of Australia and included 7889 children in school years 3–11 from government, private and Catholic schools. Data was collected from all 47 schools between August and November in 2006 with an 82% response rate. The socioeconomic status [SES] of schools was based on a written questionnaire of all families attending the school (Commonwealth Department of Education, 2005). This method of defining 85SES was considered adequate and it provided continuity of results, as it had been used in earlier studies (O’Dea, 1994; O’Dea & Caputi, 2001). Schools were categorised as being of low, middle, or high socioeconomic status (SES) based on a direct federal government measurement of parental income (Commonwealth Department of Education, Science and Training, 2005). SES status of the school community was verified by each of the state departments of education and the school principal. Total family income was assessed with 21.9% of participants from low SES schools; 58.1% middle SES schools and 20.0% high SES schools. These SES categories, were also confirmed in an interview with each of the school principals in order to verify the SES of the majority of children attending the school and the sample matches the quintile distribution of SES reported by the current Australian Bureau of Statistics social trends data for 2006 (ABS, 2006).
Participants were able to self select their ethnic/cultural background(s) from the following categories which were based on ABS Census methods (ABS, 2007): Anglo/Caucasian; Aboriginal/Torres Strait Islander; Southern European/Mediterranean; Chinese/South East Asian; Middle Eastern/Arabic; Pacific Islander; Indian; African and Other. Adequate numbers of participants to enable analyses by gender and ethnic category as well as by comparison with ABS population statistics (ABS, 2007) were recruited from Anglo/Caucasian (72.2%); Aboriginal/Torres Strait Islander (5.9%); Southern European (8%); Chinese/South East Asian (7.4%); Middle Eastern/Arabic (1.9%) and Pacific Islander (2.4%) backgrounds and these have been included in the analyses. Ethnic categories of students from African and ‘other’ backgrounds were omitted in analyses due to low numbers.
Prevalence of overweight and obesity
Prevalence of obesity was examined by age group, gender and ethnic/cultural background and these results are presented below. Analysis of obesity by gender produced no statistical differences in primary schoolchildren aged less than 12 years with 6.4% of males and 5.6% of females obese: χ2(1) = 2.16, p = 0.34. Analyses among high school students aged 12 years or older found more males were obese than females (7.7% versus 5.7%, χ2(1) = 9.13, p < 0.001).86
 87
87
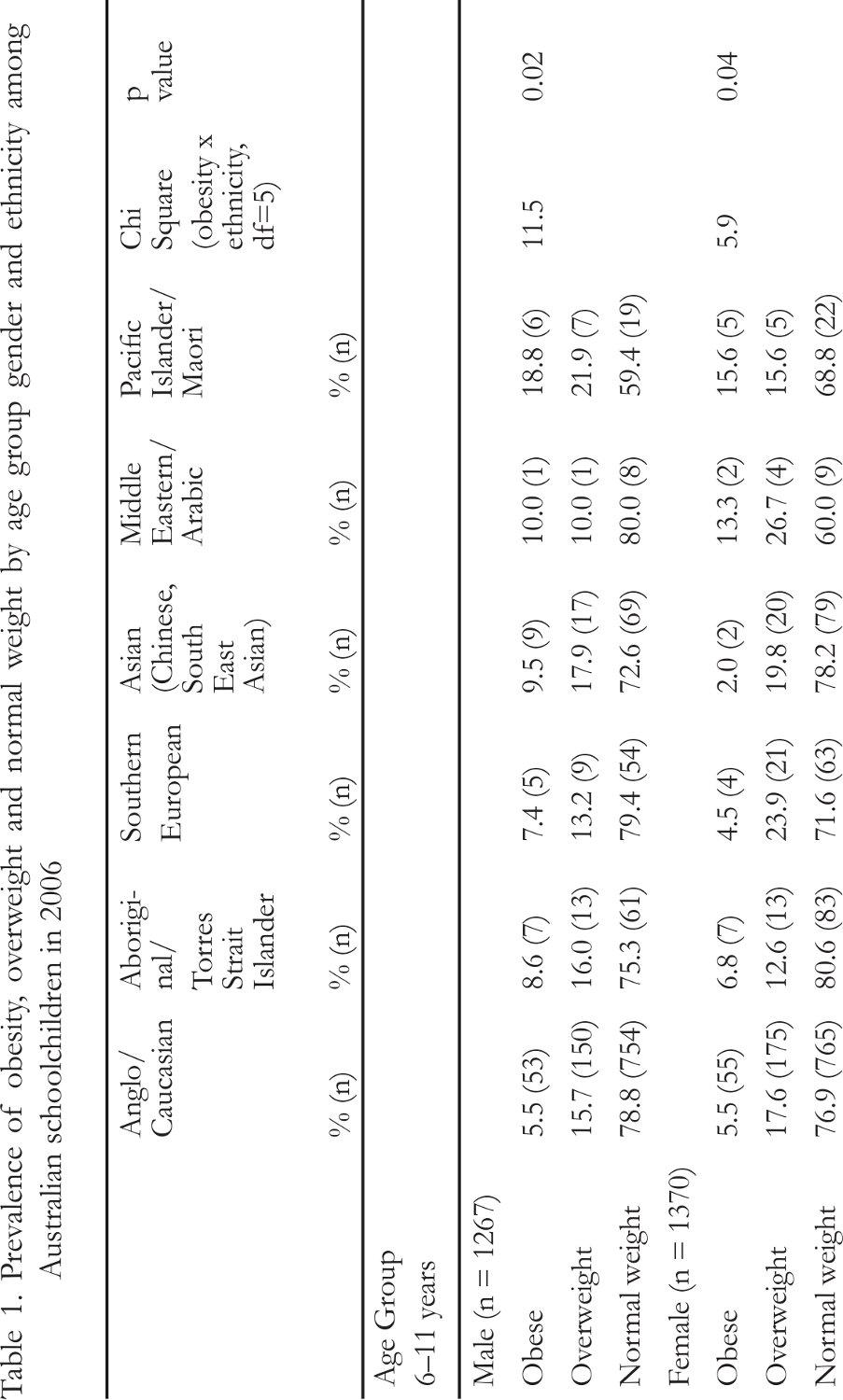
88The prevalence of obesity, overweight and normal weight by age group, gender and ethnicity among Australian schoolchildren in 2006 are given in Table 1. There was an observable and statistically different variation in obesity prevalence between different ethnic and cultural groups. Results of Chi square analyses were highly significant: χ2(10) = 134.2, p < 0.001. Differences between separate weight categories of obese, overweight and normal weight varied significantly. Obesity was significantly more prevalent among boys and girls of all ages from Pacific Islander backgrounds. Among adolescents, those who were most likely to be obese (4–5 times more prevalent, p = 0.000) were boys and girls of Pacific Islander or Middle Eastern/Arabic background. The least likely to be obese in both genders and all age groups were the Anglo/Caucasian or Asian students and in particular, the girls. Clearly, obesity among Australian schoolchildren is largely affected by ethnic and cultural factors.
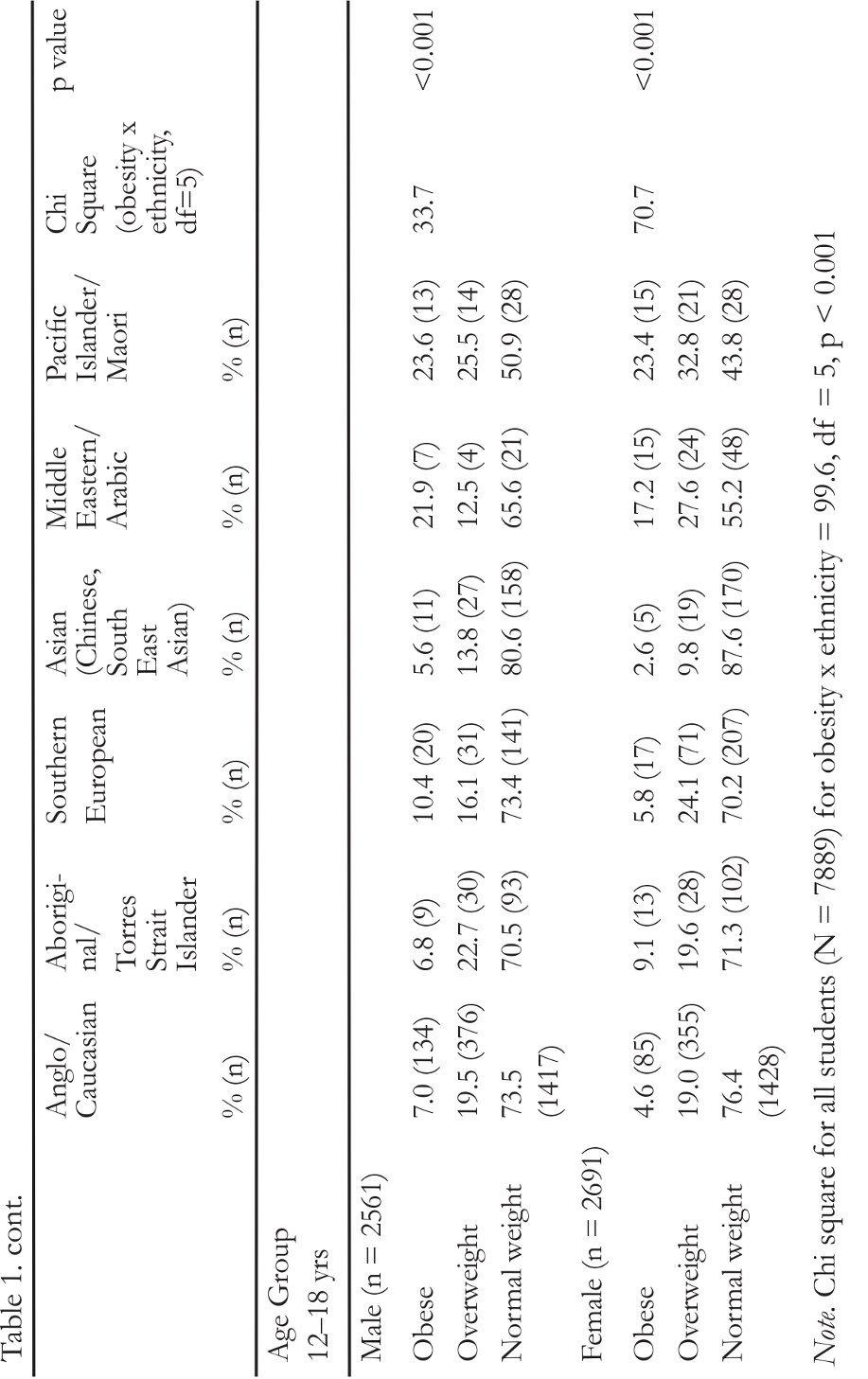
The prevalence of obesity by ethnic group is illustrated in Figure 1. Further analysis of the data also suggests a social class effect (Table 2).
The clearly graded pattern of association of obesity, overweight and SES among both primary and secondary schoolchildren suggests an influence of social class indicators upon their weight status with those of lower and middle SES having a consistently greater prevalence of obesity than their higher SES peers: χ2(2) = 25.3, p < 0.001.
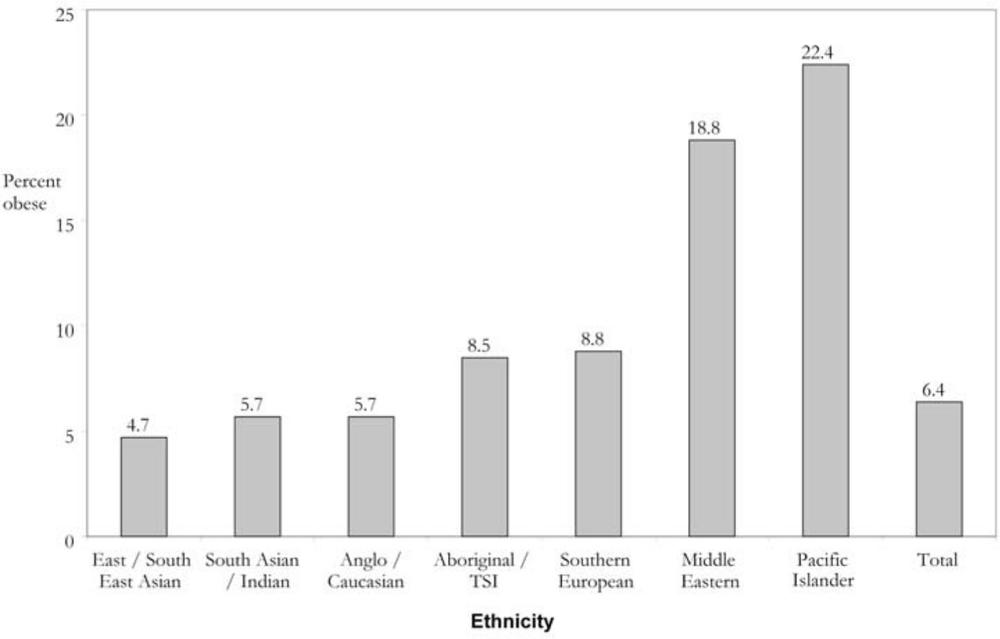
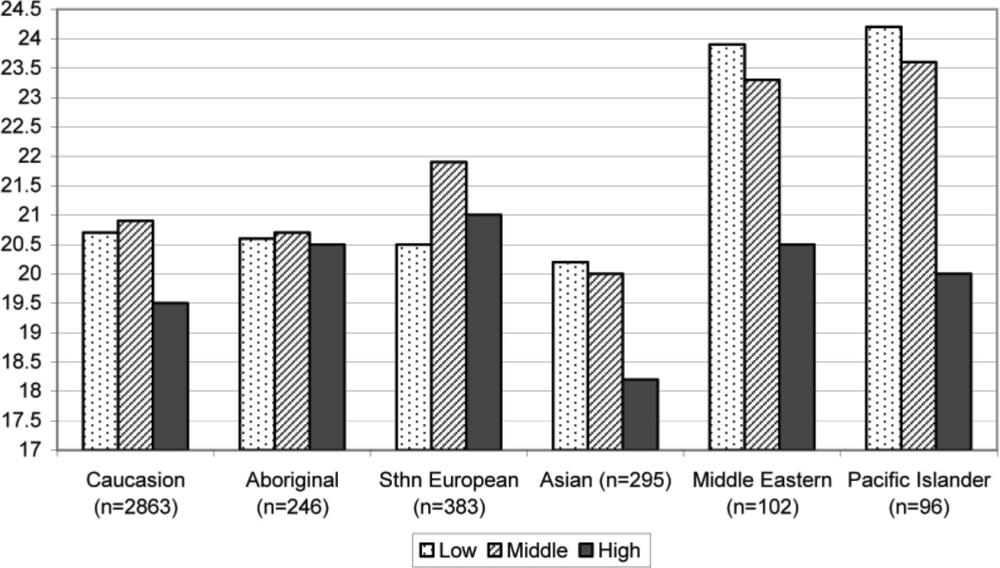
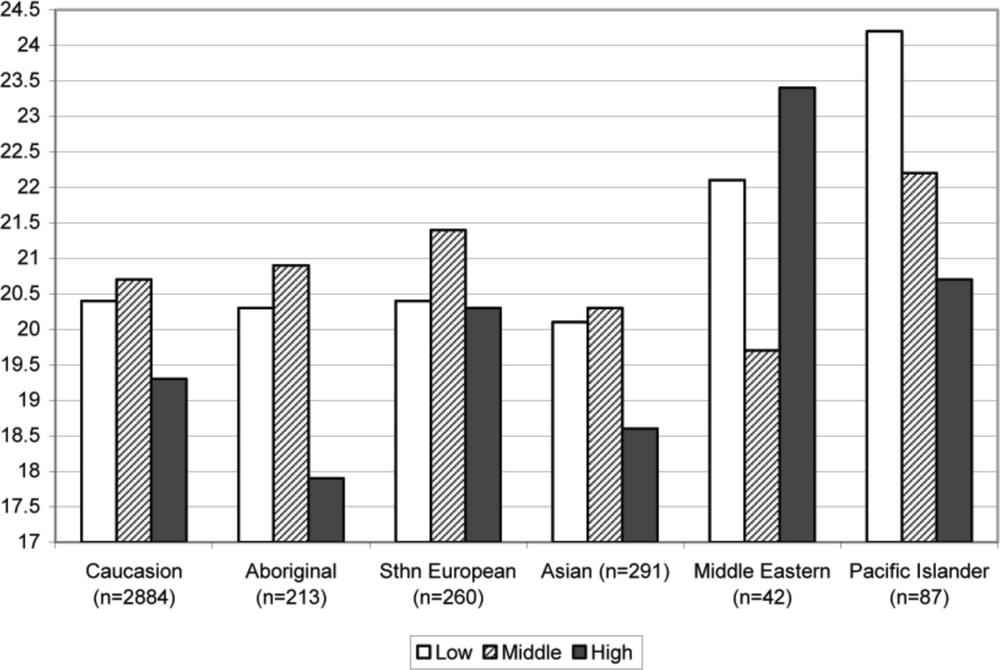
The graded effect between class and obesity is further illustrated and explained in terms of ethnicity in the following results. Whilst the trends related to SES are evident in the graphs illustrating the results of ANOVA (Figures 2 and 3), a more complex picture of the relationship between obesity and class, ethnicity and gender emerges in several ethnic groups, in which the BMI of middle SES children is much closer to that of low SES children than it is to higher SES children. There is a discontinuity between middle and higher, but not lower and middle SES for predicting BMI. This trend is particularly evident among Caucasian, Asian, Middle Eastern and Pacific Islander girls and Caucasian, Aboriginal, Southern European, Asian and Pacific Islander boys.
Among girls, (Figure 2) and after controlling for age, BMI was greater among those from Middle Eastern and Pacific Islander backgrounds compared to girls from other ethnic groups: χ2(5, 3992) = 10.46, p < 0.0001. 89
Table 2. Prevalence of obesity, overweight and normal weight by school socioeconomic status (SES) among Australian schoolchildren in 2006
| Low SES (n = 1728) |
Middle SES (n = 4583) |
High SES (n = 1578) | |
|---|---|---|---|
| Obese (n = 509) | 8.8 (152) | 6.3 (289) | 4.3 (68) |
| Overweight (n = 1458) | 19.2 (332) | 18.9 (866) | 16.5 (260) |
| Normal Weight (n = 5922) | 72.0 (1244) | 74.8 (3428) | 79.2 (1250) |
Note. Chi square test for trend for obesity x SES = 27.2, df = 1, p < 0.001; chi square test for obesity x SES = 27.3, df = 2, p < 0.001
90Girls of low SES had a generally greater BMI than girls of middle or high SES: χ2(2, 3984) = 6.22, p = 0.002.
Among boys, (Figure 3) and after controlling for age, BMI was greater among those from Middle Eastern/Arabic and Pacific Islander backgrounds compared to boys from other ethnic groups, χ2(5, 3758) = 5.78, p < 0.001. Within SES groups, boys of low SES had a generally greater BMI than boys of middle or high SES, χ2(2, 3759) = 3.92, p = 0.02.
Weight perception among obese children
The weight perception of children from different ethnic backgrounds was a crucial part of our analyses because this investigation has never been undertaken in a nationally representative sample of Australian children to date, despite several smaller studies suggesting a link between both obesity prevalence and body image among different ethnic and cultural groups. There were no significant differences in weight perceptions among obese male participants. Among obese males of all ages the number who perceived themselves to be ‘too fat’ was 58.3% Anglo/Caucasian; 50.0% Aboriginal; 56.0% Southern European; 52.6% Asian; 66.7% Middle Eastern and 55.6% Pacific Islander. The remaining percentages of boys perceived their current weight to be ‘about right’. These differences were not statistically significant: χ2(5) = 0.3, p = 0.83.
Among obese female participants of all ages the number who perceived themselves as ‘too fat’ was 68.3% of Anglo/Caucasian; 61.1% of Aboriginal; 61.9% of Southern European; 100% of Asian; 41.2% of Middle Eastern and 65.0% of Pacific Islanders. The remaining percentages of girls perceived their current weight to be ‘about right’. The differences were not statistically significant: χ2(5) = 5.1, p = 0.28.
This finding that a significant number of obese participants perceive their weight as ‘about right’ was similar but more pronounced in boys and girls aged less than 12 years.
Among obese girls aged 12 years or older, the vast majority of girls from Anglo/Caucasian (83.7%) and Asian (100%) backgrounds perceived their weight as ‘too fat’. This proportion was somewhat lower among obese girls from Aboriginal (72.7%), Southern European (70.6%), and Pacific Islander (73.3%) background, a larger minority of whom were significantly less likely to perceive themselves as ‘too fat’. However, in one group, obese Middle Eastern/Arabic girls, a majority (60%) perceived their weight as ‘about right’. The differences between the weight perceptions of ethnic groups of girls were statistically significant using a 2 by 6 Chi square: χ2(5) = 13.7, p = 0.008. The differences between obese Anglo/Caucasian girls and Middle Eastern/Arabic, Pacific Islander and Aboriginal girls were all highly significant: p < 0.001.91
Figure 1. Prevalence of obesity by ethnic group among Australian schoolchildren in 2006 (N = 7889)
Note: Graph does not include African refugees (N=53) and ‘Other’ ethnicity (N = 11) due to low numbers92
Figure 2. Mean body mass index of girls by ethnic background and socioeconomic status [ SES] (N = 2985)
93The ethnic difference between the body image perceptions of obese boys was not as clear as those differences among the same grouping of girls. Among obese boys aged 12 years or older, the percentage with a self perception of ‘too fat’ was: Anglo/Caucasian (65.7%), Aboriginal (55.6%), Southern European (61.9%), Middle Eastern (66.7%) and Pacific Islander (64.3%) boys. The differences between ethnic groups were not statistically significant using a 2 by 6 Chi square, χ2(5) = 0.92, p = 0.92.
Chi square analyses of the data among obese students by gender, SES and ethnicity revealed no statistically significant differences.
Discussion
The current study investigated the prevalence of obesity and overweight, weight perceptions and patterns of ethnic, gender and social class influences among a large, representative sample of Australian schoolchildren aged 6–18 years in 2006. The strengths of the current study include the large, nationally representative sample that includes both ethnicity and SES with a high response rate. The weaknesses include some low numbers in ethnic groups, particularly those of males from Middle Eastern backgrounds and students from India and Africa as well as the necessity to define SES using school SES rather than an individual measure of SES for each child.
In a dataset from the same survey conducted in 2000 (O’Dea and Wilson, 2006), using the international standards (Cole et al., 2000), an overall prevalence of 5.1% obesity was found, and in 2006 this had increased by 1.3 percentage points over six years to 6.4%. In comparison, the level of obesity does not appear to have increased at all among 6–12 year-old boys and girls of Anglo/Caucasian, Southern European and Asian background or 12–18 year-old girls of Anglo/Caucasian background and boys and girls of Asian background (Table 1). These findings suggest an ethnic, cultural or racial effect on the risk of obesity among children and adolescents. 94
Figure 3. Mean body mass index of boys by ethnic background and socioeconomic status [ SES] (N = 3777)
95Interestingly, whilst still showing a general upward trend, the overall prevalence of obesity does not appear to have continued to triple as suggested by earlier trends (Magarey et al., 2001). The increase in obesity prevalence of 1.3 percentage points between 2000 and 2006 (O’Dea, 2003; O’Dea & Wilson, 2006) among data from students from the same schools represents an annual increase of approximately 0.2% per year. This rate is half the rate of 0.4% per year over the 10 years reported by Magarey and her colleagues (2001) and this trend suggests a slowing of the increase in obesity prevalence and certainly defies the suggestion that childhood obesity continues to triple as it did between the 1980s and the 1990s (Magarey et al., 2001). There is also a suggestion that the obesity prevalence trend is declining in adolescent girls, especially those of higher SES and this trend has also been recently observed in another large study of schoolchildren in New South Wales (Booth et al., 2007).
These results obviously need to be further analysed and compared in more detail to determine whether the rise in childhood obesity was statistically significant, ethnically-based or related to socioeconomic status, but the trends in this study suggest that obesity is more common among low and middle SES students and those from Middle Eastern and Pacific Islander backgrounds. The prevalence of obesity in these groups of children was about 20% compared to the prevalence among children from Anglo/Caucasian backgrounds of the same age (5–7%). This finding, that obesity may be four times greater among certain ethnic groups compared to Anglo/Caucasian children, gives rise to current and future concern about the incidence of health risks, particularly insulin resistance and Type 2 diabetes among these young people.
This current result relates to other reports of Type 2 diabetes in children (Craig et al., 2007, Drake et al., 2002; Ehtisham et al., 2000; Fagot-Campagna, 2000; Sinha et al., 2002; Wiegand et al., 2004) wherein the ethnic background of the obese child, together with a family history of diabetes and a sedentary lifestyle largely predicts the prevalence of this disease. Those working with young people in clinical and community settings would be well advised to monitor obese, inactive children for the risk of Type 2 diabetes, especially if there is any family history of the disease.
An interesting finding of the current study was the apparent lack of concern and significant level of body satisfaction among obese boys. Among 96obese boys of all ages, only half considered their weight to be ‘too fat’. This may reflect a desire for ‘bigness’, muscularity, strength or masculinity among boys and young men which has been previously identified (McCreary & Sasse, 2000; McCreary, Saucier, & Courtenay, 2005; O’Dea & Rawstorne, 2001). Further research should be undertaken to establish whether this acceptance of obesity may also reflect social class mores, sporting aspirations or some other socially derived perception or desire among young males. We have also collected qualitative data which is expected to explain some of the weight related cultural beliefs and attitudes that have been identified in the current quantitative study.
The body image findings among girls were equally surprising and interesting with more than a third of the obese Aboriginal, Pacific Islander and Southern European girls seeing their weight as acceptable and possibly even desirable. This difference was marked in the obese Middle Eastern girls, nearly two thirds of whom perceived their weight to be about right and it was glaringly absent in the obese girls from Anglo/Caucasian and Asian backgrounds, with nearly all of these girls seeing themselves as ‘too fat’. These findings may reflect a way of holding on to their cultural identity in spite of the Western cultural ideal of being slim and this may be a way of balancing their need for cultural preservation with cultural adaptation.
There were measurable differences in both the prevalence of obesity and the body image and desired weight of obese children and adolescents from different ethnic groups. The body image differences of some young people in this study may reflect cultural body ideals wherein a larger body size is socially desirable for both males and females. This finding has also been recorded in studies of Fijian men and women (Becker, Gilman, & Burwell, 2005). The results also reflect widespread Western ideals of feminine beauty such as the slim ideal among Caucasian and Asian girls (Streigel-Moore, & Franko, 2002) and suggest that those children from more traditional cultures such as Pacific Island, Middle Eastern and Aboriginal cultures, may be less impacted by Westernised ideals of slimness and beauty. For some cultural groups living in Australia, fatness may remain traditionally desirable, despite their being immersed in the Western ideal of slimness.
The desire for ‘bigness’ among boys was particularly apparent, even among those who were obese and this finding is likely to reflect both traditional 97and recent Western ideals of masculinity (McCreary et al., 2005) or socially constructed gender roles (see for example, Cash & Pruzinsky, 2002; McKinley, 2002). The limitations of the BMI as an instrument of fat measurement among growing children and adolescents must not be excluded as a factor in the determination of these findings, as people from Polynesian backgrounds are known to be tall and muscular (Craig, Femia, Broyda, Lloyd, & Howard, 2007; Swinburn, Ley, Carmichael, & Plank, 1999) and it may be these factors which contribute to their weight for height, in addition to their body fat.
Whilst the prevalence of childhood obesity has been reported as increasing in Westernised countries over the past three decades (Flegal et al., 2006; Chinn & Rona, 2001) the limitations in measurement must again be clearly defined. A common, but not necessarily acceptable practice in Westernised countries is to combine children who are overweight together with those who are obese to create a category called ‘overweight and obese’. This practice ignores the fact that the categories of overweight and obesity are different because they correlate differently with percent body fat, health risk and morbidity (Flegal et al., 2006). Those working with young people must realise that whilst it is tempting to ‘advertise’ such combined statistics in order to draw attention to the health risks of obesity in children, it is not helpful or clinically accurate to combine statistics of overweight children with those who are obese.
For instance, if this limited and very simplistic definition were applied to the current study, the number of children and adolescents from Middle Eastern or Pacific Islander backgrounds who were categorised as overweight and obese would be nearly half. Clearly, this crude and clinically inaccurate measure should not be used to unnecessarily identify, stigmatise, blame or shame large children or their parents (Campos et al., 2006; Ikeda et al., 2006; O’Dea, 2004). Such methods of communicating the risk of child illness and potential disease, which may be undertaken quite innocently under the guise of ‘patient information’ or ‘community education’, may quite correctly be perceived as racially motivated, prejudiced, divisive and unhelpful among the community groups in which these weight messages are targeted. Likewise, such negatively, problem-focused messages among already socially disadvantaged groups may be seen as even more socially marginalising and victim blaming.
98Longitudinal studies of children and adolescents in the USA (Freedman, Dietz, Srinivasan, & Berenson, 1999) report higher levels of blood pressure, serum lipids and other factors associated with heart disease in adulthood but the actual risk to the child is an assumed future risk rather than a clear, valid or strong marker of current disease, ill health or ‘sickness’. Clearly, a fat child is not necessarily a sick child and this commonly held belief in Western societies is more of a myth than a scientific fact. Some would argue that the myth of ‘fatness equals illness’ is based on moralistic judgments from the protestant work ethic, wherein gluttony and sloth are assumed to reflect moral weakness, laziness and sinfulness (Gard & Wright, 2005). Consideration of biological factors in the development of obesity are also important, but the complete lack of cultural, gender and ethnic input into these narrow viewpoints of presumed ‘fatness’ is astounding.
The results of the current study may assist in a better understanding of the important interplay between these crucial socio-cultural variables by first observing the ethnic differences in obesity and body image and also weighing up the likelihood of illness, particularly Type 2 diabetes, among obese adolescents. Those who work with young people should be able to see that certain ethnic groups in Australia are both at a high risk of obesity and diabetes, but also likely to reject health education messages based on weight loss or the notion that there is something undesirable about their weight. For example, many cultures value fatness as a sign of family prosperity, fertility and success. Traditional South Pacific Islanders for example, consider ‘bigness’ or ‘obesity’ to be desirable, although fewer among the younger generation may hold these cultural perspectives (Becker et al., 2005). In order to better explain these phenomena, especially among adolescents of Middle Eastern and Pacific Islander background, we are currently analysing the qualitative focus group data from the current study.
Women and men from Pakistani and Indian backgrounds living in the United Kingdom consider the idea of spending time away from family activities and daily duties as ‘selfish’ and inappropriate, irrespective of the urgings from their doctors, nurses and other health professionals for them to undertake physical activity for the benefit of their own diabetes and their health (Lawton et al., 2006). It is likely that their children may feel the same and may adhere to similar social roles when they become adults.
99Similarly, a recent report conducted among Australian women identified several cultural barriers to women participating in sport and physical activity (Cortis & Muir, 2007).
Clearly, the challenge for nurses, health educators, community workers and other health professionals is to help people from culturally diverse backgrounds become ‘healthier’ within a broader context of their personal, family, community and cultural constructs of ‘physical, social, mental and cultural health’.
Those working in clinical, community or educational settings with young people and in particular, obese young people, should be aware that obesity is likely to be more prevalent, more culturally acceptable and perhaps more desirable among children and teens from low and middle SES communities and/or Middle Eastern, Pacific Islander and Aboriginal backgrounds. Health and social work professionals should be careful not to exaggerate the risks of obesity among higher SES Anglo/Caucasian or Asian communities as these children do not appear to be at a high risk of obesity and there is the potential to increase the risk of body image problems and disordered eating, especially among females. These different body image perceptions and socio-cultural factors should be taken into account when planning clinical, community or preventive health promotion initiatives among children or adolescents from varying ethnic groups.
References
Australian Bureau of Statistics. (2006). General social survey: summary results, Australia. Canberra: ABS, 2006.
Australian Bureau of Statistics. (2007). Year book of Australia, 2007. Canberra: ABS.
American Diabetes Association. (2000). Type 2 diabetes in children and adolescents. Diabetes Care, 23, 381–389.
Becker, A. E., Gilman, S. E., & Burwell, R. A. (2005). Changes in prevalence of overweight and in body image among Fijian women between 1989 and 1998. Obesity Research, 13, 10–17.
Blair, S. N. (2005). Activity, fitness and health outcomes in adults. American Journal of Human Biology, 19, 293–294. 100
Booth, M. L., Dobbins, T., Okely, A. D., Denney Williams, E., & Hardy L. L. (2007). Trends in the prevalence of overweight and obesity in young Australians 1985, 1997, 2004. Obesity, 15, 1089–1095.
Campos, P., Saguy, A., Ernsberger, P., Oliver, E., & Gaesser, G. (2006). The epidemiology of overweight and obesity: public health crisis or moral panic? International Journal of Epidemiology, 35, 55–60.
Cash, T., & Pruzinsky, T. (2002). Body image: a handbook of theory, research, and clinical practice. New York: Guilford Press.
Chinn, S., & Rona, R. J. (2001). Prevalence and trends in overweight and obesity in three cross sectional studies of British Children, 1974–94. British Medical Journal, 322, 24–26.
Cole, T. J., Bellizzi, M. C., & Flegal, K. M. (2000). Establishing a standard definition for child overweight and obesity worldwide: International survey. British Medical Journal, 320, 1240–1243.
Commonwealth Department of Education, Science and Training. (2005). Disadvantaged schools program: operational guidelines. Commonwealth Department of Education and Youth Affairs. Canberra: AGPS.
Cortis, N., & Muir, K. (2007). Participation in sport and recreation by culturally and linguistically diverse women. Stakeholder Consultation Report 5/07. Social Policy Research Centre, University of NSW.
Craig, M. E., Femia, G., Broyda, V., Lloyd, M., & Howard, N. (2007). Type 2 diabetes in Indigenous and non indigenous children and adolescents in New South Wales. Medical Journal of Australia, 186, 497–499.
Craig, P., Halavatau, V., Comino, E., & Caterson, I. (2001). Differences in body composition between Tongans and Australians: time to rethink the healthy weight ranges? International Journal of Obesity, 25, 1806–1814.
Drake, A. J., Smith, A., Betts, P. R., Crowne, E. C., & Shield, J. P. (2002). Type 2 diabetes in obese white children, Archives of Disease in Childhood, 86, 207–208.
Ehtisham, S., Barrett, T.G., & Shaw, N.J. (2000). Type 2 diabetes mellitus in UK children – an emerging problem, Diabetic Medicine,17, 867–871.
Fagot-Campagna, A. (2000). Emergence of type 2 diabetes mellitus in children: epidemiological evidence. Journal of Pediatric Endocrinology and Metabolism, 13, Suppl. 6, 1395–1402. 101
Flegal, K. M., Tabak, C. J., & Ogden, C. L. (2006). Overweight in children: definitions and interpretation. Health Education Research, 21, 755–761.
Flegal, K. M., Ogden, C. L., Wei, R., Kuczmarski, R. L., & Johnson, C. L. (2001). Prevalence of overweight in US children: comparison of US growth charts from the Centers for Disease Control and Prevention with other reference values for body mass index. American Journal of Clinical Nutrition, 73, 1086–1093.
Freedman, D. S., Dietz, W. H., Srinivasan, S. R., & Berenson, G. S. (1999). The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics, 103, 1175–1182.
Gard, M., & Wright, J. (2005). The obesity epidemic: science, morality and ideology. New York: Routledge.
Gracey, D., Stanley, N., Burke, V., Corti, B., & Beilin, L. J. (1996). Nutritional knowledge, beliefs and behaviours in teenage school students. Health Education Research, 11, 187–204.
Huede, B., Lafay, L., Borys, J.M., Thibult, N., Lommez, A., Romon, M., Ducimetière, P., & Charles, M.A. (2003). Time trend in height, weight, and obesity prevalence in schoolchildren from Northern France, 1992–2000. Diabetes and Metabolism, 29(3), 235–240.
Ikeda, J. P., Crawford, P. B., Woodward-Lopez, G. (2006). BMI screening in schools: helpful or harmful? Health Education Research, 21, 761–770.
Kain, J., Uauy, R., Vio, F., & Albala, C. (2002). Trends in overweight and obesity prevalence in Chilean children: comparison of three definitions. European Journal of Clinical Nutrition, 56, 200–204.
Kalies, H., Lenz, J., & von Kries, R. (2002). Prevalence of overweight and obesity and trends in body mass index in German pre-schoolchildren, 1982–1997. International Journal of Obesity Related Metabolic Disorders, 26, 1211–1217.
Kautiainen, S., Rimpela, A., Vikat, A., & Virtanen, S. M. (2002). Secular trends in overweight and obesity among Finnish adolescents in 1977–1999. International Journal of Obesity Related Metabolic Disorders, 26, 544–552.
Kumanyika, S. (1993). Ethnicity and obesity development in children. Annals of the New York Academy of Sciences, 29, 81–92.
Lawton, J., Ahmad, N., Hanna, L., Douglas, M., & Hallowell, N. (2006). I can’t do any serious exercise: barriers to physical activity amongst people 102of Pakistani and Indian origin with Type 2 diabetes. Health Education Research, 21, 43–54.
Magarey, A. M., Daniels, L. A., & Boulton, T. J. (2001). Prevalence of overweight and obesity in Australian children and adolescents: Reassessment of 1985 and 1995 data against new standard international definitions. Medical Journal of Australia, 174, 561–564. Erratum in: Medical Journal of Australia, 175, 392.
McCreary, D. R., & Sasse, D. K. (2000). Exploring the drive for muscularity in adolescent boys and girls. Journal of American College Health, 48, 297–304.
McCreary, D. R., Saucier, D. M., & Courtenay, W. H. (2005). The drive for muscularity and masculinity: Testing the associations among gender role traits, behaviors, attitudes, and conflict. Psychology of Men and Masculinity, 6, 83–94.
McKinley, N. (2002). Feminist perspectives and objectified body consciousness, pp. 55–65. In T. F. Cash & T. Pruzinsky, (Eds), Body image: a handbook of theory, research, and clinical practice. New York: Guilford Press.
McMahon, S. K., Haynes, A., Ratnam, N., Grant, M. T., Carne, C. L., Jones, T. W., & Davis, E. (2004). Increase in type 2 diabetes in children and adolescents in Western Australia. Medical Journal of Australia, 180, 459–461.
O’Dea, J. A. (2003). Differences in overweight and obesity among 4441 Australian Schoolchildren of low and middle/high socioeconomic status. Medical Journal of Australia, 179, 63.
O’Dea, J. A. (2004). Prevention of child obesity: First, do no harm. Health Education Research, 20, 259–265.
O’Dea, J. A. (2005). Improving adolescent eating habits and prevention of child obesity: Are we neglecting the crucial role of parents? Nutrition & Dietetics, 62, 66–68.
O’Dea, J. A., & Caputi, P. (2001). Socioeconomic, weight, age and gender interactions in the body image and weight control practices of 6–19 year old children and adolescents. Health Education Research, 16, 521–532.
O’Dea, J. A., & Wilson, R. (2006). Socio-cognitive and nutritional factors associated with Body Mass Index in children and adolescents: Possibilities for childhood obesity prevention. Health Education Research, 21, 796–806.
O’Dea, J. A, & Rawstorne, P. (2001). Male adolescents identify their weight gain practices, reasons for desired weight gain, and sources of weight gain 103information. Journal of the American Dietetic Association, 101, 105–107.
Ogden, C. L., Carroll, M. D., Curtin, L.R., McDowell, M. A., Tabak, C. J., & Flegal, K. M. (2006). Prevalence of overweight and obesity in the United States, 1999–2004. Journal of the American Medical Association, 295, 1549–1555.
Olshansky, S. J., Passaro, D. J., & Hershow, R. C. (2005). A potential decline in life expectancy in the United States in the 21st century. New England Journal of Medicine, 352, 1138–1145.
Padez, C., Fernandes, T., Mourao, I., Moreira, P., & Rosado, V. (2004) Prevalence of overweight and obesity in 7–9-year-old Portuguese children: trends in body mass index from 1970–2002. American Journal of Human Biology, 16, 670–678.
Rich, E., & Evans, J. (2005). The obesity discourse and body politics. Social Theory and Health, 3, 341–358.
Romon, M., Duhamel, A., Collinet, N., & Weill, J. (2005). Influence of social class on time trends in BMI distribution in 5–year-old French children from 1989 to 1999. International Journal of Obesity, 29, 54–59.
Sinha, R., Fisch, G., Teague, B., Tamborlane, W. V., Banyas, B., Allen, K., Savoye, M., Rieger, V., Taksali, S., Barbetta, G., Sherwin, R. S., & Caprio, S. (2002). Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. New England Journal of Medicine, 346, 802–810.
Streigel-Moore, R., & Franko, D. (2002). Body image issues among girls and women, pp. 183–192. In T. F. Cash & T. Pruzinsky, Body image: a handbook of theory, research, and clinical practice. New York: Guilford Press.
Swinburn, B. A., Ley, S. J., Carmichael, H. E., Plank, L. D. (1999). Body size and composition in Polynesians. International Journal of Obesity Related Metabolic Disorders, 23, 1178–1183.
Telford, R. D. (2007). Low physical activity and obesity: causes of chronic diseases or simply predictors? Medicine and Science in Sports and Exercise, 39, 1233–1240.
Wang, Y., Monteiro, C., & Popkin, B. M. (2002). Trends of obesity and underweight in older children and adolescents in the United States, Brazil, China, and Russia. American Journal of Clinical Nutrition, 75, 971–977.
Waters, E. B., & Baur, L. A. (2003). Childhood obesity: modernity’s scourge. Medical Journal of Australia, 178, 422–423. 104
World Health Organization. (2003). Obesity: preventing and managing the global epidemic. Report of a WHO Consultation Geneva. World Health Organization.
Wiegand, S., Maikowski, U., Blankenstein, O., Biebermann, H., Tarnow, P., Gruters, A. (2004). Type 2 diabetes and impaired glucose tolerance in European children and adolescents with obesity – a problem that is no longer restricted to minority groups. European Journal of Endocrinology, 151, 199–206.
Wills, W., Backett-Milburn, K., Gregory, S. & Lawton, J. (2006). Young teenagers’ perceptions of their own and others bodies: a qualitative study of obese, overweight and ‘normal’ weight young people in Scotland. Social Science & Medicine, 62, 396–406.