13
How law and regulation can add value to prevention strategies for obesity and diabetes
Steadily rising rates of overweight and obesity among adults and children in Australia and elsewhere are fuelling debate about the most effective and appropriate strategies for obesity prevention. This chapter defends a role for law in policy efforts to prevent obesity and to improve nutrition at the population level. Rather than targeting individuals and seeking to directly influence their dietary choices and patterns of physical activity, I argue that the best opportunities for law lie in improving the environment in order to support healthier choices and to reduce exposure to the wide range of factors that have made weight gain increasingly common. Secondly, this chapter presents four Australian case studies, with comparisons from the US and the UK, to illustrate the variety of priority interventions that could take legal form.
On my first day of law school, I was introduced to the law of contracts and the law of torts. In five years of lectures, however, never once did I come across the ‘law of obesity prevention’. Hitherto, preventing obesity has never been considered part of the role of law or lawyers. Lawyers have never been called on to defend the role of law in obesity prevention, or to identify the content of a package of legal interventions having that goal. The same might be said about the law of cardiovascular disease, or diabetes prevention.
Historically, public health law in Australia, Britain and the United States has been the law of unsanitary premises, abatement, and quarantine. Later, it evolved to include notifiable diseases, HIV/AIDS, tobacco control, and more recently – certainly in the United States – the law of public health emergencies and ‘pandemic preparedness’. In other respects, public health laws in all three countries have developed in a reactive and haphazard manner, reflecting successive health crises, fears and political priorities that vary between jurisdictions. Writing about English public health legislation, Robyn Martin argues that it neither has the promotion of health as its primary focus, ‘nor does it particularly address the causes of ill-health’. Instead, its focus is on inadequate premises, ‘on an understanding that ill-health results from identifiable bodies escaping from a physical source’ [1]. Only more recently, as Australian public health acts have undergone a process of renewal, has
208legislation become more proactive, and less issue-specific. South Australia’s new Public Health Act is the first such act in Australia to include specific provisions for the prevention of non-communicable conditions [2].
Quite apart from this, rising rates of overweight and obesity among adults and children have been fuelling debate about the most effective and appropriate strategies for prevention. Legal scholarship on obesity prevention, although relatively recent, is increasing in popularity, although with substantial differences that reflect the constitutional structure and political traditions of each country [3, 4, 5, 6, 7, 8, 9]. Suggested legal strategies are wide-ranging and extend far beyond the boundaries of the health sector and the traditional ‘turf’ of public health Acts.
This chapter defends a role for law in policy efforts to prevent obesity and to improve nutrition at the population level. Rather than targeting individuals directly and seeking to coerce dietary changes, or greater levels of physical activity, I argue firstly that the best opportunities for law lie in improving the environment in order to support healthier choices and to reduce exposure to the wide range of factors that have made weight gain increasingly common. This emphasis is significant: by focusing on policy, systems and environmental changes, rather than behavioural change directly, law can address the factors that shape patterns of behaviour at a population level, while avoiding the coercive and discriminatory laws to which an excessive emphasis on ‘personal responsibility’ could lead [10, 11, 12, 13].
Secondly, having set out a philosophy or framework for how law can contribute to obesity prevention, this chapter presents four case studies to illustrate the variety of legal interventions in this area. Each case study will be argued through in sufficient detail to illustrate the contested nature of legal interventions, with comparisons between regulatory developments in Australia, the US and the UK.
The trend towards population weight gain: why does it matter?
The prevalence of overweight and obesity is based on measurements of body mass index (BMI), which divides weight in kilograms by height squared (m2). In Australia, results from the 2007–2008 National Health Survey showed that 68% of men, and 55% of women were either overweight (BMI 25.0–29.9 kg/m2) or obese (BMI ≥30 kg/m2), based on measured BMI [14]. Among children aged seven to 15, almost 25% were overweight or obese, rising from 20.7% in 1995, and 11.5% in 1985 [15]. According to a Victorian government study, if current trends continue, 83% of males and 67% of females will be overweight or obese by 2025, as well as over one-third of children [16].
In Australia in 2003, cardiovascular disease (CVD) and cancer accounted for some 37% of the total burden of disease [17].2 Table 1 illustrates the extraordinary impact of modifiable risk factors on disability-adjusted life years (DALYs) from all causes in Australia, and on the leading causes of disease burden, including CVD and cancer. In 2003, overweight and obesity accounted for 7.5% of the burden of disease: almost as much as smoking (7.8%). 209
Table 1. The contribution of behavioural risk factors to the burden of disease in Australia, 2003*
| Determinant | % of DALYS (all causes)# | % of DALYS (specific causes)^ |
| Tobacco | 7.8% | 20.1% of cancer |
| High blood pressure | 7.6% | 42.1% of CVD |
| Overweight & obesity | 7.5% | 19.5% of CVD |
| Physical inactivity | 6.6% | 23.7% of CVD |
| High blood cholesterol | 6.2% | 34.5% of CVD |
| Alcohol harm | 3.3% | 3.1% of cancer |
| Alcohol benefit | –1.0% | –4.7% net benefit on CVD |
| Lack of adequate fruit, vegetable intake | 2.1% | 9.6% of CVD |
* Begg S, Vos T, Barker B, Stevenson C, Stanley L & Lopez A (2007). The burden of disease and injury in Australia, 2003. Canberra: AIHW. PHE 82 (p74).
# Disability-adjusted life years
^ Contribution of each risk factor is independent of other risk factors (analysis is not additive)
Overweight and obesity are risk factors for high blood pressure, raised cholesterol, impaired glucose tolerance, a range of chronic conditions including CVD (coronary heart disease and stroke), type 2 diabetes, a variety of cancers (including colon, breast and ovarian cancer), as well as gallbladder disease, osteoarthritis, gout, and sleep apnoea [18]. Many of these conditions are exacerbated by high blood pressure (for which excess salt consumption is a risk factor), high blood cholesterol (for which excess consumption of saturated fat is a risk factor), and inadequate intake of fresh fruit and vegetables. According to one estimate, in 2007, around 24% of type 2 diabetes, 21% of cardiovascular disease, 25% of osteoarthritis, and 21% of colorectal, breast, uterine and kidney cancer were attributable to obesity [19].
In the US, the prevalence of obesity (defined as BMI >30 kg/m2) remained relatively stable from 1960 to 1980 but climbed sharply thereafter, from 15% in 1976 to 1980, to 34% in 2007–2008 [20, 21]. Over the same period, obesity in children and adolescents (aged two to 19 years) tripled from over 5% to 17% [22]. Overall calorie intake, mean intake from carbohydrates, and absolute fat intake also increased over this period [23, 24]. Some epidemiologists warn that increases in BMI in the US, and its impact on diabetes, CVD and other conditions, will increasingly outweigh the positive impact on life expectancy of declining smoking rates, and could cause a decline in life expectancy at birth and at older ages during the first half of this century [25, 26, 27]. In Australia, D’Arcy, Holman and Smith have warned that, based on recent trends in population weight gain, by the time they are 20, the life expectancy of Australian children will fall two years, pulling them back to 2001 and 1997 levels for males and females, respectively [28].210
In 2010, Colagiuri and colleagues estimated the total direct costs of overweight and obesity in Australia in 2005 at A$21 billion, with an additional A$35.6 billion spent by government on pensions and subsidies [29]. Between 2003 and 2033, treatment costs for type 2 diabetes are estimated to increase by 520%, from A$1.3 billion to A$8 billion, largely driven by the impact of rising obesity rates on diabetes prevalence [30]. In the US, by 2008, annual medical costs attributable to obesity are estimated to have reached US$147 billion [31]. In 2007, RAND Corporation estimated that if current trends continue, by 2020 up to one-fifth of all healthcare expenditures could be obesity related [32].
Debates about the right policy approach to population weight gain
The susceptibility of individuals to weight gain is influenced both by non-modifiable factors such as age, sex and genetics, and by modifiable dietary and physical activity patterns. Modifiable factors contributing to energy oversupply include the frequency and energy value of the food eaten (fat and alcohol contain more calories per gram than protein and carbohydrates), and the duration and intensity of physical activity. On the other hand, obesity is also a population issue: the weight distribution of the population as a whole has drifted steadily to the right over the past two decades.
The rapid changes in national obesity rates over the past few decades suggest that it is environmental influences upon average eating and physical activity patterns within the population that explain the epidemic, rather than individual or genetic factors [33, p118]. Previous generations shared our genes and physiology, but rates of obesity were lower. Explaining the trend towards weight gain solely in terms of people eating too much and exercising too little is self-evident, but ignores the impact of environmental and policy factors on changes in average behaviour, and hence the causes of the trend itself. The temptation to explain an emerging epidemic, such as obesity, purely in terms of the private choices of individuals also obscures the contribution of corporate behaviour (such as the food industry) to population health trends, as well as the responsibility of governments to create the conditions for a healthy lifestyle. Understanding this is critical if we are to develop an effective response.
If Australians, as a population, were to adopt a healthier lifestyle, there is little doubt that life expectancy, and healthy life expectancy, could dramatically increase. For example, the INTERHEART study found that over 90% of the risk of heart attack in men and women, young and old, across all geographical regions and ethnic groups, could be predicted by eight risk factors, several of which are certainly modifiable [34]. These are: smoking, physical inactivity, obesity, high blood pressure, high blood cholesterol, diabetes, inadequate fruit and vegetable intake, and psychosocial stressors.
Knowing this, however, is not enough. As the trend towards weight gain illustrates, people find it difficult to eat healthily and to maintain energy balance. In a survey of over 150 000 Americans, 76% were non-smokers, 40% had a healthy weight, 23% had the appropriate intake of fruit and vegetables, and 22% exercised regularly. But only 3% of the sample were following all four of these healthy lifestyle factors [35]. One of the authors of the 211study said: ‘The effect of following these [lifestyle guidelines] is greater than anything else medicine has to offer. I don’t know anything a doctor’s office can do that would reduce your risk of diabetes or cardiovascular disease by 80% or 90%’ [36]. In Australia, Atlantis and colleagues found that while 55% of Australians are eating enough fruit, less than one in four were meeting national guidelines for physical activity (a minimum of 2.5 hours per week of moderate-intensity physical activity, including walking, spread across five or more days per week). Less than 15% were meeting eating enough vegetables, and less than 5% were doing all three [37].
Faced with policy challenges as complex and contested as obesity, there is a temptation for governments in liberal, market-oriented societies – facing coordinated pressure from food and beverage manufacturers and retailers – to frame the problem as one that individuals face. The answer seems blindingly obvious: every individual should exercise more ‘personal responsibility’. In well-quoted comment, Australia’s former health minister, the Hon. Tony Abbott MHR said:
It is estimated that obesity adds about a billion dollars a year currently to the nation’s health bill. Obviously I would rather that we didn’t have to spend that money … but in the end if people are obese it’s because they’re eating too much or they’re exercising too little, and the answer is in the hands of those individuals [38].
This is wise counsel – for individuals. However, as a conceptual framework for reducing national healthcare costs and the burden of disease caused by obesity and diabetes, it will continue to fail.
Unless motivational strategies and health promotion can magically unlock new personal resources for healthy living that are not already being tapped by the weight-loss industry, or neutralised by the variety of influences in modern societies that make healthy living difficult (such as time poverty, long commutes, loss of cooking skills, food marketing and the ubiquity of cheap, unhealthy food), then this is a counsel of despair. Governments are often attracted to health promotion campaigns using mass media, which were an effective tool in tobacco control strategies. As Wakefield and colleagues point out, however, media campaigns are likely to be more successful when the behaviour that needs to be changed is ‘one-off or episodic’. This is not the case with healthy eating and physical activity, which requires sustained discipline and daily effort, well after the campaigns have ended (39]. Furthermore, the norms about ‘normal weight’ are changing. Surveys indicate that males and females in the US [40] and the UK [41], and Australian males [42] do not perceive their (over)weight accurately. Unless individuals recognise when they are overweight, they may have little reason to alter their lifestyles.
To summarise so far: taking responsibility for health is an excellent idea for individuals. However, populations cannot necessarily be expected to ‘take responsibility’ or to ‘shape up’ in the way that individuals (sometimes) can. Mass media campaigns are part of a comprehensive policy response, but governments need to be realistic about what they can achieve. To arrest the population-wide trend towards weight gain, we need to address 212factors to which the population as a whole is exposed: the social forces that shape the way people live [43].
Where does law and regulation fit with obesity prevention strategies?
Most models for understanding the causes of health and disease recognise that health outcomes are the result of a complex interplay of environmental, socioeconomic, biological and individual behavioural factors, partially modified by interactions with the healthcare system (Figure 1) [44]. Strategies for obesity prevention tend to reflect different assumptions about the relative importance of the policy, systems and environmental factors that lie outside of the individual, the behavioural factors that are the individual, and the biological and genetic influences that lie within the individual. The discussion above has already pointed out the limitations of strategies that focus narrowly on the behavioural domain, relying on mass marketing to encourage personal responsibility and motivationally led, self-directed changes in behaviour. As discussed below, each of the strategic domains set out in Figure 1 – the environment (from global to local level), individual behaviours, and the health system – provide opportunities for regulatory interventions that could contribute to healthier eating and improvements in physical activity at a population level. The challenge for public health lawyers is to identify law reform priorities and to make the case for those interventions which are best implemented through legal and regulatory processes.
(i) Regulating the healthcare system
Population growth and the ageing of the population mean that Australia’s healthcare system will face a higher burden of chronic disease in future. In 2008, for example, over one million Australians had type 2 diabetes, and over 242 000 of them had it as a result of being obese (an increase of 137% over 2005 figures) [19]. Law plays a crucial role in improving the effectiveness of clinical care; for example, by creating stable rules for the sharing of patient data within an electronic health records system that enjoys public trust, yet permits optimal access to a patient’s data at all points of care. In Australia, important elements towards achieving this include the development of a personally controlled electronic health records service [45], which builds on the Healthcare Identifiers Service that uniquely identifies individuals and healthcare providers [46, 47].
In a bold experiment, New York City extended notifiable disease reporting to chronic disease risk factors, through the mandatory reporting of haemoglobin A1c (glycated haemoglobin, a measure of blood glucose control). By making diabetes a notifiable disease, the New York City Department of Health and Mental Hygiene is creating a registry that will map the epidemiology of hyperglycaemia and help to facilitate care for the estimated one-third of diabetics who are unaware of their condition [48, 49, 50].3 Although controversial
213[51], this initiative deserves careful study elsewhere. Due to the frequent co-location or clustering of chronic disease risk factors in the same individual [52, 53, 54], the New York City law could assist in identifying other risk factors for chronic disease in individuals who – not coincidentally – tend to be of lower socioeconomic status [55, 56, 57]. Ironically, it is this capacity for chronic disease risk surveillance to potentially contribute to reducing health inequalities that also enables this strategy to be framed as discrimination against poor people of colour.
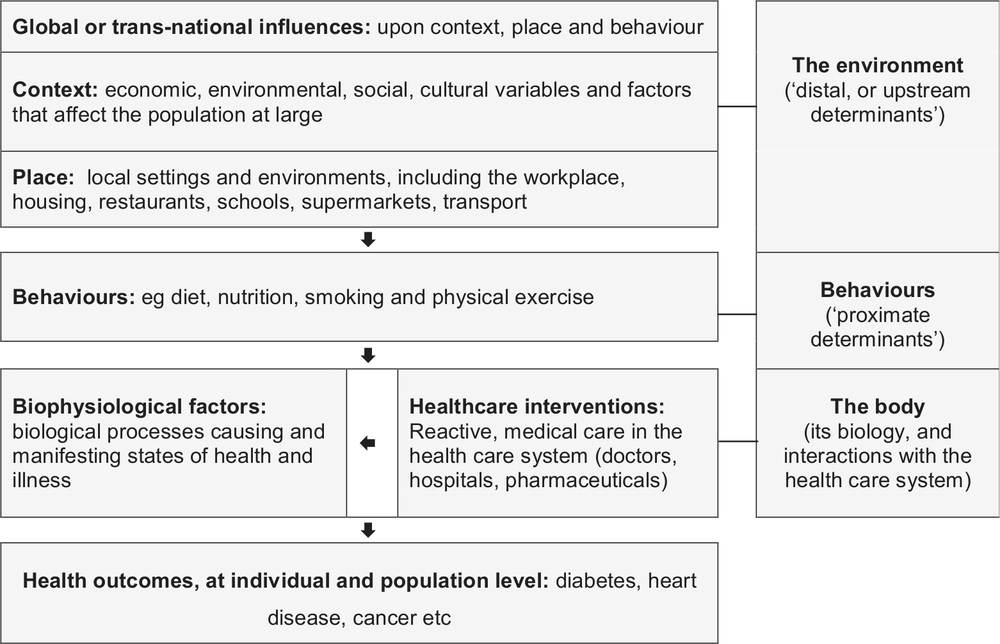
Figure 1. A simplified, hierarchical model of the determinants of health and disease
In addition to improving diagnosis and treatment, regulation can enhance the process of integrating secondary prevention within primary healthcare systems. The Australian Government has taken several initiatives in this direction, including the introduction of new Medicare item numbers providing reimbursement for general practitioners to carry out medical check-ups on patients aged from 45 to 49 who present with identifiable risk factors for chronic disease, and patients aged from 40 to 49 whose risk factors (including excess weight) put them at risk of developing type 2 diabetes [58].4 In its comprehensive review of strategies for chronic disease prevention, the National Preventative Health Taskforce recommended that the Medical Benefits Schedule should support prevention through practice-level incentive payments or payments to individual medical practitioners to support brief interventions and a followup consultation directed to tobacco, alcohol,
214obesity, or other risk factors for chronic disease [59, p260]. In the UK, pay-for-performance contracts have been a feature of general practice reform; a substantial proportion of GP income depends upon ‘quality points’ that are earned when practice targets are met, including those for the assessment and management of risk factors for heart disease, asthma and diabetes [60, 61]. Unlike Australia, patient registration with local NHS practices facilitates continuity of care and a stable patient group for measuring performance.
In Australia, the Practice Incentive Program currently supports performance-based incentive payments to general practices for the successful management of diabetes patients, amongst other areas [62, 63]. The Australian Primary Care Collaboratives program also supports primary practices to improve their capacity to manage and reduce risk factors in the patient group, and to improve management of chronic and complex conditions [64, 65].
From July 2011, the Australian Government began to roll out a network of independent, primary healthcare organisations, known as Medicare Locals [66]. Building on the existing Divisions of General Practice, Medicare Locals identify service gaps and develop formal and informal linkages to integrate the care provided by different service providers. Their role also includes the delivery of health promotion and risk prevention programs targeted to the risk profiles of local communities [67, pp8, 48].
(ii) Targeting the behaviours of individuals
Many people would intuitively understand legal strategies for obesity prevention as crude attempts at behaviour modification, whether through education, financial incentives and disincentives, or more direct forms of control. More benign interventions include evaluative food labelling initiatives which, quite apart from encouraging reformulation by food manufacturers, aim to alter purchasing patterns by educating consumers about the nutrient qualities of foods. Less benign interventions that might be seen as ‘targeting’ the behaviour or weight status of individuals include restrictions on taxpayer-funded medical procedures for obese patients and smokers [68, 69, 70], or the elimination of community rating resulting in differential premiums for private health insurance, and other restrictions in coverage, based on one’s obesity or health status.
In April 2008, Japan introduced a legal requirement on companies and local governments to measure the waistlines of Japanese people aged from 40 to 74 as part of their annual check-up. Japan has adopted official limits for waistlines – 33.5 inches for men, and 35.4 inches for women, based on International Diabetes Federation estimates for identifying health risks. Companies and local governments that fail to meet targets for measuring waistlines will be fined [71]. These policies raise the question of who should bear responsibility for the rising prevalence of lifestyle risk factors, including obesity, not to mention the ethics of intruding into the lives of individuals and discriminating against them based on weight [10, 11, 12].
Imposing an additional tax on high-fat or high-salt foods, or eliminating tax concessions for novated vehicle leases, illustrate policies that aim to ‘nudge’ behaviour in a healthier direction by increasing the costs of unhealthy choices and regulating in order to make the healthy choice the ‘default option’ [12, 72]. These policies are defended on the basis 215that people find it difficult to make choices that are consistent with their longer-term preferences and welfare, for reasons that include limited willpower, inadequate information and cognitive constraints, and social and cultural influences, including advertising [12, 73]. People are also overoptimistic, preferring current consumption while discounting its future, adverse impacts on them personally [74].5 On the other hand, policies can subtly shape patterns of choice within populations in ways that are not necessarily mediated through the conscious deliberations of individuals. Interventions of this kind are best understood as being directed at the broader environment, rather than at individuals.
(iii) Improving the quality of the economic, social, physical and policy environment
Although debate persists about the underlying drivers of energy imbalance and weight gain, economic factors are crucial [75, 76]. Relevant factors include the reduced cost of food (particularly energy-dense carbohydrates), and the growth of a commercial food sector marketing processed snack foods (leading to an increase in snacking). Pre-prepared and pre-packaged foods are ubiquitous and heavily marketed, and manufacturers compete for market share by satisfying human preferences for energy-dense, fatty, salty, and sweet foods. Boyd Swinburn points out that the trend towards population weight gain is evidence of commercial success [77], although weight gain brings longer-term costs that the industry externalises. In addition to the changing food culture, technological change has resulted in high levels of car use, and less need for both incidental physical activity and arduous work. Entertainment is frequently passive; not surprisingly, there is a correlation between overweight and hours spent watching television [78].
Scholars point out that population weight gain is, in fact, a normal response to these environmental influences upon diet and physical activity patterns [76]. Two factors follow. Firstly, if the causes of population weight gain lie in the environmental domain, then mitigation ‘require[s] socioeconomic, not health sector reforms’ [76, p12]. A feature of so-called population health approaches to obesity prevention is the emphasis on interventions that address these ‘upstream’ environmental and socioeconomic determinants. As Geoffrey Rose stated, a population health approach ‘attempts to remove the underlying causes that make the disease common’ [79]. To the extent that this can be done successfully, a population health approach has the capacity to shift ‘entire risk factor distributions at the population level, not simply the causes of cases at the individual level’ [80].
On the other hand, this does not mean that obesity prevention is the process of identifying and seeking to reverse the factors that plausibly explain the population trend. Not only would it be impossible to reverse the processes of economic development and globalisation that have given us higher incomes, labour-saving devices, television, pre-prepared food, and a higher proportion of women in the paid workforce, it would also be highly undesirable. Rather than return society to the Stone Age, the policy priority is to identify
216feasible, evidence-informed and culturally acceptable ways of counteracting the impacts of an ‘obesogenic’ environment. Necessarily, this involves finding ways of effectively achieving population nutrient intake goals: reducing salt, fat and free sugars, improving intake of fibre and fresh fruit and vegetables, and increasing levels of physical activity [81].
I would argue that the best opportunities for law lie in addressing the socioeconomic and environmental factors that are driving the increase in average weight gain. ‘Privatising’ the obesity epidemic – confining it to the healthcare setting, or emphasising personal responsibility to the exclusion of everything else – is unlikely to reverse the trend. Until policy-makers focus on the influences to which populations are exposed, there will be nothing to prevent the occurrence of new cases [33, p178]. On the other hand, to the extent that societies are successful in creating supportive environments that encourage healthier lifestyles, it will be ‘less necessary to keep on persuading individuals’ [79]. By using legal and policy levers to alter the obesogenic environment, the goal is to ‘outweigh’ those environmental contributors to energy imbalance that it is not feasible to change. An environment that better supports healthier choices and lifestyles will also be a more fertile ground for education strategies and health promotion, and for targeted strategies pursuing behaviour change and significant weight reduction among high-risk groups [82, 83, 84, 85].
A final point to make is that where the absolute risk of the population is too high – because, for example, average weight, salt or saturated fat intake is too high – it is not the case that the only ones to benefit from prevention policies are those who have the highest relative risk by virtue of being on the far right hand tail of the distribution. The risk of diabetes, for example, rises modestly with BMI within the normal range, and exponentially at higher levels [86]. Although interventions may benefit the smaller number of people at highest risk, the greatest benefit may be among the much larger number of people in the middle part of the disease distribution who are exposed to a relatively low risk [33, pp176–78, 87].
The importance of a ‘plausible policy basket’
Before suggesting some law reform priorities for obesity prevention, a dose of realism is needed. No society has yet succeeded in reversing the future reservoir of disease and healthcare expenditure that population weight gain will produce [88]. Given the tenacity of many of the conditions that currently contribute to poor diet and sedentary lifestyle – from long working hours and lack of time, to geographically dispersed suburbs – multiple policy changes will be needed. Implementing a sufficiently broad basket of policies through the political process will be extremely challenging, and incremental progress is the most likely scenario. Nevertheless, serious action on obesity prevention is needed now, before things get worse, relying on the best available evidence, monitoring the entire basket of policies, and adding promising new ones as they become feasible. Insisting on cast-iron evidence of effectiveness for each new policy is an invitation to policy paralysis. Sensibly, the National Preventative Health Taskforce called for a ‘trialling of a package of interventions’ accompanied by monitoring and evaluation: a ‘learning by doing’ approach [67, p92].217
Scholars including Anjali Jain have pointed out that since there are multiple determinants of population weight gain, ‘solutions are also likely to be multifactorial, with no single intervention providing widespread success. Thus it is less important to isolate why an approach is successful, than it is to find interventions that work’ [89, p1388]. It is the combined impact of a basket of ‘plausible interventions’ that is likely to make a difference: no single policy is likely to deliver a ‘king hit’. At the same time, it is the complex and multi-factorial nature of population weight gain that makes law reform a constant struggle. In so far as policy-makers seek to regulate individual behaviours in ways that move beyond education and advice-giving, they run the risk of offending civil libertarians. In so far as they adopt a population health perspective and move upstream, seeking to influence the social and economic determinants of obesity and chronic disease, they risk offending the free marketeers. Since a population-wide approach necessarily seeks to achieve changes in the behaviours of large number of people, policies will inevitably have an impact on those who do not perceive themselves to be at risk and who may resent the ‘interference’. Selling temperance is difficult at the best of times, and becomes even harder when the food industry unites in opposition to a proposed policy initiative, decrying the lack of evidence, in circumstances when the scale of the benefit to public health is unknown, despite its likely value as part of a package of interventions. Critics fume that public health should stick to what it knows best: communicable diseases control, and keeping bugs out of the food supply. They resent public health becoming a smokescreen for interference in the market economy, or for policies to redress health inequalities by re-shaping the political economy [90, 91, 92, 93].
Obesity prevention and the struggle for regulatory control
Ultimately, law’s role in chronic disease and obesity prevention boils down to the exercise of raw political power. As Stephen Leeder points out, ‘It’s war’ [94]. Underlying reasons for opposing the use of law and regulation as tools for obesity prevention are not difficult to uncover. Firstly, obesity is neither contagious, nor readily transmitted to others (notwithstanding evidence that obesity – probably through its behavioural antecedents – spreads through social ties over significant periods of time) [95]. It follows that the justification for interfering with individual preferences in order to protect the population from health risks to which it has not consented, is absent.
Secondly, the goal that underlies at least some interventions for obesity prevention involves reducing consumption, whether it be total calories, the amount of saturated fat in the diet, or the habit of snacking. The interests of the food and beverage industry, on the other hand, lie in avoiding policies that could de-stabilise revenue flows based on consumer preferences and markets – as shaped by industry.
Thirdly, obesity prevention strategies are often vulnerable to attack by economic conservatives and libertarians who frame the prospect of any regulation – even controls on advertising and clearer nutrition labelling – as evidence of ‘nanny state’ interference with 218the personal autonomy of consumers and parents [90, 91, 92, 93, 96, 97].6 The Hon. Tony Abbott MHR stated in 2006:
I don’t think we can put people in cotton wool. I don’t think we can cover our population in cling-wrap. I think people need to retain substantial authority over how they live their lives … I think the role of the Government, in this instance at least, is not so much to regulate, let alone to ban. I think its role is to encourage, to inform and to give good example [98].
An alternative view would acknowledge that governments are stewards of the health of the population, and have a responsibility to invest in policies that support healthier lifestyles in ways that do not unduly burden individual freedom. To the extent that governments acknowledge this responsibility, a population health approach offers important advantages. By targeting the influences upon – and influencers of – behaviour, rather than the behaviour itself, regulatory interventions can contribute to health improvement without stigmatising individuals, or micro-managing their lifestyles [99]. Success in tobacco control, for example, came about while substantially preserving the liberty of adults to smoke where this does not jeopardise the health of others [100].
The obstacles to effective obesity prevention law reform are not only ideological. Effective structures for facilitating a comprehensive, inter-sectoral approach do not even exist. Government agencies have their own entrenched cultures: it can be difficult to collaborate with them, difficult to usurp their turf, and difficult to route around them. Political leadership is required from the top, and federalism complicates everything [101, 102]. With this in mind, the remainder of this chapter reviews four case studies for legal and regulatory interventions to support obesity prevention.
Priorities for law and regulation in the prevention of population weight gain
So far, I have argued that a sustainable approach to reversing the trend towards population weight gain calls for a ‘plausible policy basket’ that focuses significantly – not necessarily exclusively – on creating environments that better support physical activity and healthy eating. Piecemeal, ad hoc responses are unlikely to have a major impact, due to the combined force of the many factors that subtly encourage excess energy intake and a sedentary lifestyle.
The strategies that law can deploy as a tool to prevent obesity and to encourage an active lifestyle can be described in different ways [5, 6, 7, 8]. Gostin’s well-known model [103] includes:
- laws that shape the informational environment, for example, mandatory front-of-pack nutrition labelling [104], restaurant calorie labelling of ‘standard food items’ [105, 106, 107], and laws restricting the advertising of energy-poor, nutrient-poor foods to children;
- economic policies that alter the costs of behaviour, such as taxes on sugary, fizzy drinks [108, 109]; 219
- laws that shape the physical environment, for example, through infrastructure investment, planning controls on the density of fast food outlets [110], or New York City’s ‘green cart’ permit scheme to increase the availability of fresh fruit and vegetables [111, 112];
- social policies to address social disparities, for example, subsidising the freight costs of fresh fruit and vegetables to remote indigenous locations [67, pp134–35]; and
- prescriptive controls on business; for example, bans on the use of trans fats [113].
Each of these examples illustrates ways in which regulation can change the ‘external’ environment. In addition, however, regulation has an ‘internal aspect’, which refers to governance initiatives whose focus is institutional reform, and structures for improving the strategic and organisational capacity of government to respond to health challenges. This is the focus of the first of four case studies, below.
(1) Improving governance structures for cross-sectoral collaboration and policy leadership
Goal: To deliver an inter-sectoral, whole-of-government approach to policy development for obesity prevention
In 2008 to 2009, Australia’s federal government spent A$112.8 billion on health, but only 2% of this (A$2.3 billion) was spent on public health [114]. At present, public health functions compete for funding within health departments that are focused on treating the sick. In addition to the difficulty of achieving more adequate investment, however, lies the challenge of achieving a voice in policy development in sectors beyond health. In the context of obesity prevention, this means a voice in policies relating to transport and urban development, local government, agriculture and food (production, manufacture, retail, catering, advertising), education, and taxation [115]. Achieving an inter-sectoral, all-of-government approach to strategy, policy and program development is perhaps the most important priority for taking innovative and incremental steps that could reduce the burden of disease, and healthcare expenditures, in Australia’s ageing population.
Developing architecture to support an inter-sectoral approach to policy development requires strategic choices, including between an essentially government-focused, and a community-focused structure. One model is a ‘politically owned’ governance structure with a mandate – secured through high-level (preferably cabinet-level) leadership and support – to forge cross-departmental links and to develop an integrated response that is consistent with the government’s commitment to act. This model might include inter-departmental taskforces or standing committees that provide the opportunity for relevant ministries to consider the negative impact of their policies and programs on shared health goals, as well as opportunities for a more coherent, all-of-government approach.
The National Obesity Prevention Act of 2008, a federal bill introduced into the 110th US Congress, illustrates the first kind of structure [116]. This bill would have established an inter-Departmental Task Force, supported by an Advisory Committee on Obesity, with a 220mandate to develop a government-wide strategy for obesity prevention, supported by goals for each agency, with a requirement for each agency to review its budgets and programs and to determine their impact on physical activity, nutrition and obesity rates. The bill would also have required each agency to report annually on its implementation of the national strategy and its impact on obesity rates.
Although this bill was never passed, its essential structure is reflected in President Obama’s more recent National Prevention, Health Promotion and Public Health Council [117], which recently published the National Prevention Strategy [118] and is tasked with monitoring the policies of a dozen federal agencies, reporting annually on progress towards the goals in the strategy, and suggesting corrective actions to agencies to assist them to achieve the goals. In the UK, the Blair government adopted a multi-sectoral approach to health inequalities, setting out the commitments, key actions and spending required for each department as part of the all-of-government strategy. Importantly, the strategy was overseen by a Cabinet sub-committee chaired by the deputy prime minister [119].
An alternative model for supporting an inter-sectoral approach is an independent-of-government structure that is less constrained by party politics, but nevertheless has a clear mandate to advise on policy options. On the one hand, the benefits of this second model include its independence from the entrenched cultures and agendas of existing departments, its likely capacity to engage more effectively with consumers, business, and the NGO sector, and its ability to perform functions governments might wish to avoid, such as evaluating industry practices. On the other hand, this remoteness and lack of political power could limit the effectiveness of such a body in genuinely influencing the policy agenda of departments and in raising the profile of possible solutions.
A third model of particular relevance to Australia is a ‘portfolio agency’ with a statutory mandate that lies outside the health department, but within the health portfolio, with executive leadership reporting directly to the minister.7 With adequate resources and a statutory mandate, such an agency may be able to move more effectively between departments and to assume the role of ‘honest broker’, while engaging effectively with business and community groups. The functions of the CEO of the recently established Australian National Preventive Health Agency include encouraging partnerships with industry, non-government organisations, and the community sector; developing standards and codes of practice relating to preventive health matters; advising the minister, and publishing a biannual report on the state of preventive health in Australia. If requested to do so, the CEO can also make recommendations about preventive health to the federal health minister, to the Australian Health Ministers’ Conference, to state and territory governments and the Australian Local Government Association [120]. It seems clear, however, that the functions of the new agency have been designed to prevent it from interfering in departmental policies or in the political sphere, as distinct from engaging in health promotion and on non-legislative and voluntary actions by business and within the community sector.
221In 2009, the National Preventative Health Taskforce proposed a Prime Minister’s Council for Active Living driving the development and implementation of a National Framework for Active Living encompassing transport, the built environment, and social engagement [67, pp99–100]. The aim was that the Prime Minister’s Council would develop a business case for consideration by the Council of Australian Governments for a new funding partnership that would link future infrastructure funding in these areas to the agreed outcomes for active living. This recommendation was rejected on the grounds that the National Preventive Health Agency, and other existing mechanisms including Medicare Locals and the national Partnership Agreement on Preventive Health, could deliver appropriate outcomes [59, pp34–35].
Chronic disease prevention competes with many other issues for the attention and resources of cabinet, ministers and departments. The easier option, as reflected in the National Preventive Health Agency, is to create agencies to lead efforts to encourage behavioural change by individuals through mass media campaigns and voluntary actions. Important as they are, these investments need to be matched by governance structures that facilitate serious consideration of how all ministries and sectors can shape their policies in order to encourage and even privilege healthier food choices and a more physically active lifestyle.
(2) Reducing or eliminating advertising of high-sugar, high-salt, high-saturated-fat (HSSF) foods to children
Goal: To reduce or eliminate diet-distorting commercial influences on children’s diets due to the relentless marketing of energy-dense, nutrient-poor foods; to reduce ‘pester power’ and to support parents in exercising personal responsibility to provide a healthy diet for children
The exposure of children to television advertising of energy-dense, nutrient-poor foods has become a litmus test for the willingness of governments to use regulation to create a healthier food environment for children [121]. Evidence suggests that Australian parents are concerned about food advertising to children and support stronger regulation [122]. On the other hand, due to assumptions about personal responsibility and commercial freedom, reducing food advertising to adults is not seriously on anyone’s agenda, even where constitutional constraints do not preclude it. Overweight and obese children are more likely to remain so in adulthood [123], and to the extent that unhealthy food advertising could be reduced, it would not only assist parents to exercise parental responsibility to provide a healthier diet for children, but would create incentives for the food industry to improve the nutrition of leading products, or to re-direct advertising dollars towards healthier foods.
In Australia, evidence continues to demonstrate that energy-dense, non-core foods are heavily advertised during children’s peak television viewing times [124, 125, 126]. In the US, in 2006, 44 food companies spent over US$1.6 billion promoting food and beverages to children and adolescents, predominantly carbonated beverages, quick-serve restaurant food and breakfast cereals [127].
Although there is a positive association between the amount of television watched and increased consumption of commonly advertised foods, and between exposure to television 222and obesity, both for adults [128, 129] and children [78, 130, 131, 132], the argument that this link is mediated by the impact of food advertising depends upon a distinct chain of reasoning. For children, this includes the assertion that food advertising alters preferences and purchase requests [133], which attach to higher-energy, advertised foods that crowd out and replace the more energy-dilute foods the child would have eaten if not exposed to advertising. While it is logical to assume that ‘fast-food restaurants would not choose to advertise if advertising did not increase the demand for their products’ [134], proving a causative link – as distinct from demonstrating correlations between a cluster of behaviours – has not been straightforward. In a recent paper, Boyland and colleagues reported that children preferred to select high-fat and high-carbohydrate foods after viewing food commercials, and that this effect was more pronounced among children who were habitual television viewers [135]. The authors point out that their findings support the argument that food advertising not only alters brand choice but alters generic food preferences in favour of energy-dense, nutrient-poor foods.
A consistent theme in food advertising is the presence of voluntary, industry-designed schemes that are promoted as accommodating community concerns about childhood obesity and obviating the need for direct government involvement. In the US, evidence suggests that as a result of pledges made under the Council of Better Business Bureau’s Children’s Food and Beverage Advertising Initiative [136], television food advertisements viewed by children aged two to 11 declined by 12% between 2004 and 2008. However, by 2010, exposure to food advertising increased by 9% over 2008, and in 2010 children viewed 39% more ads for fast food and other restaurants than in 2002 [137]. Adolescent exposure to food advertising increased by 23% during 2004 to 2010; adult exposure increased at an even higher rate [138]. Another study found that in 2009, over two-thirds of all food advertising by signatories to the Children’s Food and Beverage Advertising Initiative was for non-core (‘once-in-a-while’) foods, and that healthy food advertising was invisible [139].
In 2009, the US Congress authorised an appropriation to establish the Interagency Working Group on Food Marketed to Children comprising representatives of the Federal Trade Commission (FTC), Food and Drug Administration, the Centers for Disease Control and Prevention, and the Department of Agriculture. The working group was tasked with developing a set of food marketing principles to guide industry self-regulation that would improve the nutritional profile of food marketed to children aged two to 17 years [140]. From 2016, the working group’s proposed principles would require all food products falling within the ten most heavily marketed product categories to comply with two nutrition principles. These set maximum values for ‘negative’ nutrients including saturated fat, added sugars and sodium, and secondly, require all marketed foods to ‘provide a meaningful contribution to a healthful diet’ by containing minimum amounts of either fruit, vegetables, whole grains, low-fat milk or a number of other food categories [140]. Although the final principles are voluntary, they will represent a credible consensus of relevant federal agencies on permissible forms of food advertising to children, which these agencies will expect the food industry to implement by 2016. If the food marketing principles are widely ignored, this could encourage the FTC to explore the full reach of 223its powers to regulate food marketing to children (subject to First Amendment, tailoring and evidential challenges) and theoretically, could provide support for the restoration of the FTC’s rule-making powers under the unfairness doctrine [141]. By setting normative standards, engaging with the food industry, and monitoring and reporting on its compliance, the FTC could encourage both improvements in food marketing practices, and the reformulation of heavily advertised foods.
In its submission to the Interagency Working Group in July 2011, the Children’s Food and Beverage Advertising Initiative (CFBAI) announced new uniform nutrition criteria, to be implemented by 31 December 2013, which define the nutritional characteristics for foods advertised to children under 12 across ten product categories [142]. Arguing that the Interagency Working Group’s proposed principles are ‘not realistic and thus … not aspirational’ [143], the CFBAI argued that the application of the Interagency Working Group’s principles to children and adolescents aged two to 17 is ‘overly broad and inappropriate’, whereas the CFBAI ‘properly focuses on advertising primarily directed to children under 12’ [143, p23].
Australia’s co-regulatory approach to children’s food advertising begins with the Children’s Television Standards 2009 (CTS) prescribed by the Australian Communications and Media Authority (ACMA) [144, 145]. The CTS apply to the designated children’s (C) and preschool (P) programming that broadcasters are required to broadcast under their licences (CTS 6–19). Compliance with the CTS is a license condition for commercial television broadcasters [146]. The CTS provide that where advertisements contain premium offers, such as toys offered for sale with advertised foods, the advertisement must not make reference to the premium ‘in a way that is more than merely incidental’ to the advertised product (CTS 33(2)). The CTS prevent the repetition of advertisements within any 30-minute period (CTS 29), and prohibit the promotion of commercial products by popular characters, including animated, cartoon and movie characters (CTS 35). Food advertisements may not contain misleading or incorrect information about the nutritional value of the product (CTS 32(7)).
Evidence suggests that food advertisers have regularly ignored the CTS in the past [147, 148]. In a review of the 2005 version of the CTS, completed in 2009, ACMA decided against imposing any additional restrictions on food advertising during children’s designated programming, concluding that ‘the relative contribution of advertising to childhood obesity is difficult to quantify and the causal relationship between these may not be possible to determine’ [149, p9]. ACMA also carried out economic modelling which showed that banning the advertising of foods high in fat, salt or sugar (HSSF foods) could significantly affect the revenues and profitability of broadcasters [149, p6]. As Ingleby and colleagues point out, the revenue consequences of restricting unhealthy food advertising ‘becomes less attractive as a proposition when it is translated into an argument that children should be exposed to harm as the price of having television programs made for them’ [150].
The Children’s Television Standards are supplemented by the co-regulatory Commercial Television Industry Code of Practice [151] which is registered as a code of practice under the Broadcasting Services Act 1992 [152]. This code provides that food advertisements 224directed to children shall not promote an unhealthy lifestyle, or the excessive or compulsive consumption of foods or beverages [151, para 6.23]; it also requires compliance with the Code for Advertising & Marketing Communications to Children adopted by the Australian Association of National Advertisers (AANA Code) [153]. Neither code is designed to restrict the frequency, timing or placement of advertisements for energy-dense, nutrient-poor foods directed to children [154]. Leaving aside the fact that both codes rely wholly on consumer complaints, and lack independent monitoring, both codes also consist of generally expressed principles which recent practice suggests are exceedingly difficult to break. Neither code restricts the cumulative impact of unhealthy food advertising on children’s preferences and expectations [154, pp134–38].
As evidence and community concern about food marketing to children have continued to grow, the food industry has sought to manage the political risk of regulation by developing additional self-regulatory schemes. Recent initiatives include the Responsible Children’s Marketing Initiative developed by the Australian Food and Grocery Council (AFGC) [155], which came into operation during the period when ACMA was reviewing the Children’s Television Standard (2005). The AFGC Initiative applies to designated children’s and preschool programming, and G-rated programs where >50% of the audience are children under 12 years, but not other programming where children are nevertheless a significant share of the audience. In 2009, when the National Preventative Health Taskforce recommended phasing out the marketing of energy-dense, nutrient-poor (ENDP) food on free-to-air and pay TV before 9pm, together with premium offers and the use of competitions, cartoons and promotional characters, the Australian Government responded that it would continue to monitor the effectiveness of voluntary codes including the AANA Code, the AFGC Initiative, and a similar initiative by the Quick Service Restaurant Industry [59, pp46–47].
King and colleagues evaluated non-core food advertising before and after the introduction of the AFGC’s Responsible Children’s Marketing Initiative. They found that while signatories to the AFGC initiative reduced their rate of non-core food advertising, there was no reduction in the rate of non-core advertisements overall (which continue to dominate peak viewing times), since non-signatories to the initiative increased their rate of non-core food advertising [124]. Nor should it be assumed that exposure would be dramatically reduced if more advertisers implemented the AFGC principles, given their focus on programs directed to children, rather than children’s peak viewing periods. Hebden and colleagues found that the introduction, in August 2009, of the children’s marketing initiative of the Quick Service Restaurant Industry made no difference to the frequency of non-core fast food advertisements broadcast during peak children’s viewing periods [156].
Handsley and colleagues have argued that if the goal is to actually reduce children’s exposure to non-core food advertising, restrictions based on time of day will be required, not merely restrictions on advertising within designated children’s programming [157]. In the UK, broadcast advertising is regulated by the UK Code of Broadcast Advertising (BCAP Code), which was written and is reviewed by an industry body, the Broadcast Committee of Advertising Practice (BCAP) under delegation from OfCom, the telecommunications 225regulator [158, 159]. In 2006, the Food Standards Agency (FSA) advocated a complete ban on all advertising of foods high in salt, sugar and fat on television before 9pm [160]. After a lengthy inquiry, OfCom did implement a ban on HSSF food advertising [158, section 32.5], based on the nutrient profiling model developed by the FSA [161]. The ban applies specifically to advertising of foods high in salt, sugar and fat in ‘programmes commissioned for, principally directed at or likely to appeal to’ audiences below the age of 16. OfCom has contracted out the enforcement of the BCAP Code to the Advertising Standards Authority [162].
The significant difference between ‘children’s programs’ or ‘programs targeted at children’, and ‘peak children’s viewing periods’ illustrates the political and philosophical difficulty of implementing an effective ban, which would require the value of commercial speech to adults to be balanced with the benefits of encouraging healthier diets for children and adolescents. Other important variables include whether advertising restrictions apply to children and adolescents, or only to children; the nutritional parameters of foods that attract any ban; and whether or not the administering authority is a government agency, industry or independent body. While there is substantial evidence in Australia showing that the food advertising children are exposed to does not support a healthy diet, governments are reluctant to take on the food industry, and regulation will only improve things to the extent that it addresses the criteria above.
(3) Economic incentives to encourage investment in workplace-based risk prevention and health promotion programs
Goal: To exploit the workplace, in both the private and public sectors, as a setting for disease prevention and health promotion programs encompassing smoking cessation, obesity prevention and healthy eating
Although calls for a ‘fat tax’ are regularly made and are the best-known example of an economic strategy for obesity prevention [163], there is a wide range of options for altering the policy environment in ways that could indirectly influence food consumption patterns at the population level. These include imposing a levy on television advertising of energy-dense, non-core foods that do not meet minimum nutritional criteria [164], eliminating the tax deductibility of food advertising costs for non-core foods [134], as well as financing initiatives to make fresh fruit and vegetables more accessible and affordable to lowincome and remote populations [165]. In 2010, the Australian Government rejected the recommendation of the National Preventative Health Taskforce to commission a review of economic policies, including the use of taxation, grants, pricing, incentives and subsidies to promote access and consumption of healthier foods and greater levels of physical activity [59, p37]. The wide-ranging Henry review of Australia’s future tax system also rejected the notion of a fat tax, because of the difficulty of accurately estimating the health and productivity costs attributable to particular (less healthy) food or product constituents, and because of the multiple influences – besides food choices – on obesity, including genetic, social and economic factors [166]. The population health effects of the dietary changes that could result from a tax on certain classes of food or food ingredients are also not well understood [167].226
Like schools, and healthcare encounters, the workplace is an important setting for disease prevention. A growing body of research evaluates the business case for workplace-based disease prevention and health promotion programs, and seeks to identify the optimal design elements, spending and managerial requirements of successful programs [168, 169]. Since risk reduction and better employee health offers the promise of reductions in future healthcare costs and sick leave, and improved productivity and morale, workplace-based risk prevention programs provide the opportunity for alignment between the economic goals of business, the public health goals of government, and the interests of individual employees. At the global level, the World Economic Forum hosts the Workplace Wellness Alliance and promotes corporate wellness initiatives as an opportunity for multinational companies to contribute to the prevention of chronic disease [170, 171].
In the US, employers have a direct financial incentive to invest in evidence-based wellness programs, not only because absenteeism and low productivity affect the bottom line, but also because employees’ health insurance premiums are typically paid for or are heavily subsidised by employers. In 2010, 69% of non-federal private and public employers offered health benefits to employees. Of these, nearly three-quarters of employers offered ‘wellness programs’. Services typically included in these programs include: weight-loss and smoking cessation programs, personal health coaching, gym membership discounts, nutrition and healthy living classes, and online resources [172, p170]. Increases in healthcare premiums, including employee contributions [172, pp20–21], combined with the economic downturn and the imperatives of deficit reduction, are driving a longer-term trend towards government policies to encourage workplace-based health promotion programs, with sharper financial incentives for employees to participate in them. For employees, this typically means submitting to a health risk assessment, followed by the development of an individualised risk reduction program, with annual review.
President Obama’s Patient Protection and Affordable Care Act (PPACA), signed in 2010, authorises grants to small businesses (<100 employees) to establish comprehensive wellness programs [173], and provides for the development of reporting requirements for group health plans to report on wellness and health promotion initiatives, including smoking cessation, weight management, diabetes management and nutrition [174]. It also requires the Centers for Disease Control and Prevention to conduct a periodic national survey of workplace-based health programs and to provide technical assistance to employers in evaluating such programs [175].
Federal law currently restricts employers from varying health insurance premium contributions according to the health status of the particular employee [176]. However, an important exception permits premium discounts or rewards of up to 20% of the cost of the employee’s premium contribution where the employee has complied with the requirements of a wellness program that is ‘reasonably designed to promote health or prevent disease’ [177, 178]. From 2014, this incentive is increased to 30%, and up to 50% if the Secretaries of Health and Human Services, Labor and the Treasury so determine [179, 180]. The point at which financial incentives for participation in wellness programs (in both private and state-funded health insurance schemes) become intrusive and coercive, remains a matter of 227debate [181]. From 2014, the PPACA guarantees the availability and renewability of health insurance cover for employers and individuals, prescribes the grounds on which premiums may vary, and further restricts discrimination based on an individual’s health status [182]. PPACA requires all plans to include an ‘essential benefits package’ (including specified preventive and wellness services and chronic disease management) [183], and sets up a number of risk adjustment processes to allocate payments to plans with high-risk enrolees. In this environment, the central role of health promotion and risk prevention programs in reducing healthcare costs, with financial incentives to encourage participation, seems set to continue.
One bill not passed by Congress in 2009 would have offered tax credits to businesses setting up comprehensive wellness programs, for a period of ten years [184]. One of the primary goals of the US-based Workplace Wellness Alliance is to ‘develop and advocate for tax-credit and other legislation that promotes worksite health promotion programs and other health management initiatives’ [185].
The twin factors that are helping to drive investment in wellness programs in the US – that is, the direct financial burden on employers who either self-insure or pay the larger share of employees’ health insurance premiums, coupled with financial incentives for employees – are absent in Australia. Australians enjoy taxpayer-funded, rather than employer-funded, national healthcare coverage through Medicare, and private health insurance is community rated [186]. Any reversal of community rating would likely undermine the market for private health insurance and increase demand for Medicare-funded services, something the Australian Government would be keen to avoid.
In 2009, the National Preventative Health Taskforce argued that public sector organisations at all levels of government should lead by example by introducing, identifying and replicating successful workplace-based health promotion programs that could serve as ‘models of good practice to the employment sector as a whole’ [67, p53]. To encourage uptake within the private sector, they suggested that health promotion programs should be exempt from fringe benefits tax, free of goods and services tax (GST), and tax deductible. The Australian Government did not respond directly to these recommendations, although it has indicated it does not support exempting employer-funded smoking cessation programs from fringe benefits tax [59, p73].
From 1 July 2011, under the National Partnership Agreement on Preventive Health [187], the Commonwealth is providing up to A$289 million in funding to the states to develop healthy living initiatives in the workplace [188]. The NSW Healthy Workers Initiatives, for example, will comprise advice, support and resources for businesses (including a website, phone service and onsite assistance), as well as a coaching service for individuals [189]. For its part, the Commonwealth is developing a National Healthy Workplace Charter with peak business groups, national standards, and an awards scheme for best practice in workplace health programs.
Despite the differences in health insurance arrangements, the US experience has clear implications for Australia. The workplace offers a rare opportunity for a win–win partnership 228between government, business and public health stakeholders, yet what is absent are economic drivers. Australian employers are largely protected from the direct healthcare costs of employee ill-health, and unless there is compelling evidence to demonstrate that a healthy workers initiative dramatically improves productivity in the short to medium term, uptake is unlikely to be on the scale required to substantially contribute to disease prevention goals. What the current voluntary model overlooks is that workplace-based initiatives are not merely a vehicle for improving business productivity by enlightened businesses; rather, the workplace is an important setting for reaching a large proportion of the working population.
This suggests two priorities. Firstly, the Australian Government should act on the recommendation of the National Preventative Health Taskforce by reconsidering how the taxation system could best support the uptake of healthy worker programs, encompassing smoking cessation, obesity prevention and improved nutrition. Secondly, governments, as employers, should lead by example, implementing comprehensive programs for the benefit of government employees, and using their purchasing and contracting powers to impose accreditation standards to drive improvements in the nutritional quality of foods sold in government buildings, hospitals and other public sector settings.
(4) A co-regulatory approach to food reformulation
Goal: To moderate overconsumption of saturated fat, sugar and salt at the population level by providing a statutory underpinning to food reformulation negotiations encompassing food manufacturers, retailers, government, and public health stakeholders
The availability of ‘cheap, palatable, energy-dense foods’ that are skilfully marketed and high in fat, sugar or salt, is an important change in the environment that has driven the upward trend in population weight gain over the past few decades [190]. Reformulation of food products is a population-level ‘superpolicy’ that could improve nutrition by reducing the amount of overconsumed nutrients. Some major food manufacturers and retailers, such as Pepsico [191] and Wal-Mart [192], are already taking steps to improve the nutritional profile of their portfolio of products.
Prevailing beliefs about the importance of free markets, limited government regulation, consumer choice and personal responsibility support the view that it would be inappropriate for a government agency to prescribe mandatory standards for nutrients (salt, sugar, saturated fat) for the food sector. A competing view might hold that regulation has a legitimate role to play in setting the ground rules for a multi-stakeholder process to drive nutritional improvements within the food supply. There are several factors that, in combination, suggest a growing role for government in public health nutrition.
Firstly, although the status of good nutrition, as a value within Australian food regulation, remains ambiguous, anyone familiar with the Food Standards Code cannot fail to acknowledge that nutrients in food are already regulated prescriptively and in almost forensic detail, in order to reduce health risks, to set parameters for health and nutrient claims, and to avoid confusion, misunderstanding and deceptive advertising [193].229
Secondly, consumers cannot make healthy choices in circumstances where only a minority of products (for example, snacks and beverages) meet ‘healthy’ nutritional criteria [194] and where there is no evaluative food labelling scheme to assist consumers to rapidly distinguish between products based on their nutrition [104]. Thirdly, in the light of evidence of its role in cardiovascular disease, New York City, followed by a range of US states and cities, has banned trans fats in restaurant cooking [195, 196].
Over time, salt reduction also has the potential to significantly re-shape assumptions about the legitimate limits of food regulation. Around three quarters of salt intake in most high-income countries comes from added salt in processed foods and pre-cooked meals [197]. This eliminates choice and, since most individuals are unaware of their high-salt intake, hampers personal efforts to moderate consumption. The benefits of salt reduction in controlling hypertension and reducing cardiovascular disease at the population level is strongly supported by evidence, but requires gradual – and more than trivial – reductions in salt levels across those product categories that most contribute to excess levels [198, 199]. Many countries have adopted voluntary targets for reductions in population salt intake, managed by government [200] or, as in Australia, through a Food and Health Dialogue that includes government, the food industry and public health groups [201]. A measure of resistance (passive or active) to substantial reductions in salt targets, by at least some sections of the food industry, is predictable. For example, evidence suggests that salt reduction will reduce sales of sugar-sweetened soft drinks (which could assist in obesity prevention) [202]. Habituation to highly salty foods encourages demand for cheaply produced, profitable snacks, while water-binding chemicals in combination with salt can increase the water content, and thus the weight, of meat [199, pp377–78].
In 2009, the UK government set voluntary targets for salt reduction for the food industry to meet by 2012 [203], while New York City is coordinating a National Salt Reduction Initiative that includes 44 cities and states [204]. In Australia, the National Preventative Health Taskforce recommended that the Australian Government establish a Healthy Food Compact to drive changes in the food supply, with voluntary targets for reductions in salt, saturated and trans fats, and sugar [67, pp106–09, 144]. In a muted response, the Australian Government has committed A$900 000 over three years to ‘develop the evidence base and rationale for future food reformulation activities’ under the existing, voluntary, Food and Health Dialogue [59, pp38–40].
There is growing academic interest in regulatory strategies for reducing salt intake at the population level [205, 206]. In 2010, the Institute of Medicine recommended that the Food and Drug Administration revoke the ‘generally recognised as safe’ status of salt and set mandatory national standards for added salt to foods. These would be implemented in a step-wise manner, allowing consumer taste preferences to adapt and industry to resolve technical challenges [207].
One way of ensuring that food reformulation negotiations achieve an adequate level of momentum is through a co-regulatory approach that adds a statutory underpinning to what is currently a purely voluntary process. Consistent with the prevailing model of 230‘responsive regulation’ – which favours ‘soft’, voluntary measures and only escalates to more direct forms of regulation and enforcement when voluntary strategies fail [67, pp57–58] – participation in the food reformulation dialogue could remain voluntary. In the absence of significant levels of participation from major food manufacturers and retailers, however, a voluntary process would stall. In that event, there should be a credible expectation that government will intervene more directly.
While the key components of a co-regulatory framework require further elaboration, they might begin by enshrining a Healthy Food Compact as a public process with a formal existence recognised in legislation or, at a minimum, in a code of practice developed by an appropriate host agency, such as the Australian National Preventive Health Agency [208] or Food Standards Australia New Zealand [209]. The code of practice could set out the goals of the dialogue for a defined five-year period, together with the roles, and respective obligations of government, manufacturers, retailers and industry associations, and community-based organisations, as participants in the dialogue. Major food manufacturers and retailers whose market share exceeds a prescribed minimum would be expected to become signatories to this process.
Signatories might also be offered choices; for example, between making prospective, binding commitments to reduce average levels of salt, saturated fat, and energy across priority food categories, and to increase levels of fibre and fruits, vegetables, nuts and legumes – versus participation in the dialogue for the relevant five-year term. Prospective commitments might be preferable for signatories that wish to maximise flexibility as well as reduced scrutiny of their product portfolio and manufacturing processes. Under the negotiated process, signatories would need to negotiate towards feasible targets for improvements in the nutrition of products within priority product lines against a credible expectation that if target levels were not achieved, default levels in some areas might be set through a government-appointed process. Progress would be monitored with public reporting.
While the focus of negotiations across the various priority categories within the food reformulation dialogue would be improved nutrition, the focus of negotiations involving retailers could involve commitments relating to the advertising and marketing of healthy foods, and increased visibility and shelf space for healthier products. Both streams would rely on the goodwill of those involved to work effectively: government, manufacturers, industry associations, consumer groups, and experts in public health and nutrition. The ground rules for the dialogue would need to balance public health goals with technical feasibility and consumer acceptability, pursuing significant change across the food supply, while minimising damage to existing brands.
Conclusion
I have argued in this chapter that governments have a critical role to play in the prevention of obesity and diabetes through the development of a ‘plausible policy basket’ that includes both regulatory and non-regulatory interventions. Significant improvements in health and wellbeing, not to mention productivity, are unlikely unless governments acknowledge 231this leadership role. Effective policies for obesity prevention require governments, in collaboration with other stakeholders, to recognise that improving the public’s health is a legitimate goal for public policy, rather than delegating responsibility for health to individuals and private markets. At the same time, there is plenty of scope for reasonable people to disagree about the legitimate boundaries of law reform initiatives, since public health policies are difficult to keep separate from political philosophies.
Although a multi-level response is needed that addresses environments, lifestyles and healthcare services, the case studies presented in this chapter – governance reform, food advertising controls, incentives for disease prevention within the workplace, and a clearer structure for commercial food reformulation – are all directed at the environment, rather than at individuals and their behaviours per se. While this will not satisfy the critics, there is an important distinction here. Personal autonomy remains an important value in free, market-oriented societies. On any fair assessment, the case studies presented here do not involve dictating lifestyles or diets to individuals.
On the other hand, policies that create a more supportive environment for healthy living may very well conflict with the economic interests of those businesses that derive substantial revenues from current patterns of overeating, poor nutrition and physical inactivity. In tobacco control, public health advocates have learned that there are few, if any, opportunities for collaboration with tobacco companies [210, 211]. From a perspective of two or three decades, however, legislatures have literally driven over the top of the tobacco industry, dramatically reducing the scale of tobacco use (if not the profitability of tobacco companies themselves) in the process. Reducing the ‘food economy’ is not the goal of obesity prevention. On the other hand, it would be naive of the food industry, looking towards the next decade or so, to assume that governments will not seek to offset rising healthcare costs and stagnating productivity by experimenting with regulatory measures to reduce the preventable component of chronic disease. While debate continues about whether the food and beverage industries can be genuine partners in strategies to improve diet and reduce energy intake [191, 212, 213, 214, 215], the point is that the law of obesity prevention has already arrived and is likely to stay for some time. Its future remains to be written, debated, implemented and evaluated. That said, regulatory interventions, like those presented in the case studies above, may come sooner than many expect.
References
1. Martin R (2001). Domestic regulation of public health: England and Wales. In R Martin & L Johnson (Eds). Law and the public dimension of health (pp75–112). London: Cavendish (p79).
2. South Australian Public Health Act 2011 ss. 61–62.
3. Reynolds C (2004). Law and public health: addressing obesity. Alternative Law Journal, 29: 62–167.
4. Mello M, Studdert D & Brennan T (2006). Obesity: the new frontier in public health law. New England Journal of Public Health, 354: 2601–10.232
5. Monroe J, Collins J, Hon. P.Maier, Merrill T, Benjamin G & Moulton A (2009). Legal preparedness for obesity prevention and control: a framework for action. Journal of Law, Medicine & Ethics, 37(Suppl. 1): 15–23.
6. Pomeranz J & Gostin L (2009). Improving laws and legal authorities for obesity prevention and control. Journal of Law, Medicine & Ethics, 37: 62–75.
7. Sacks G, Swinburn B & Lawrence M (2009). Obesity policy action framework and analysis grids for a comprehensive policy approach to reducing obesity. Obesity Reviews, 10: 76–86.
8. Magnusson R (2008). What’s law got to do with it? Part 1: a framework for obesity prevention. Australia and New Zealand Health Policy 2008 [Online]. Available: www.anzhealthpolicy.com/content/5/1/10 [Accessed 20 October 2011].
9. Magnusson R (2008). What’s law got to do with it? Part 2: legal strategies for healthier nutrition and obesity prevention. Australia and New Zealand Health Policy 2008 [Online]. Available: www.anzhealthpolicy.com/content/5/1/11 [Accessed 20 October 2011].
10. Wikler D (2002). Personal and social responsibility for health. Ethics & International Affairs, 16(2): 47–55.
11. Leichter H (2003). ‘Evil habits’ and ‘personal choices’: assigning responsibility for health in the 20th century. The Milbank Quarterly, 81: 603–26.
12. Le Grand J (2008). The giants of excess: a challenge to the nation’s health. Journal of the Royal Statistical Society Series A, 171: 834–56.
13. Jesson J (2008). Weighing the wellness programs: the legal implications of imposing personal responsibility obligations. Virginia Journal of Social Policy and the Law, 15: 217–98.
14. Australian Institute of Health & Welfare (AIHW) (2010). Australia’s Health 2010. Canberra: AIHW (p114).
15. Roberts L, Letcher T, Gason A & Lobstein T (2009). Childhood obesity in Australia remains a widespread health concern that warrants population-wide prevention programs. Medical Journal of Australia, 191: 46–47.
16. Victorian Department of Human Services (2008). Future prevalence of overweight and obesity in Australian children and adolescents, 2005–2025, Melbourne: Department of Human Services.
17. Begg S, Vos T, Barker B, Stevenson C, Stanley L & Lopez A (2007). The burden of disease and injury in Australia, 2003. Canberra: AIHW, (p39).
18. Kim S & Popkin B (2006). Commentary: understanding the epidemiology of overweight and obesity – a real global public health concern. International Journal of Epidemiology, 35: 60–67.
19. Access Economics Pty Ltd (2008). The growing cost of obesity in 2008: three years on. Report by Access Economics Pty Ltd to Diabetes Australia.
20. Flegal K, Carroll M, Ogden C & Johnson C (2002). Prevalence and trends in obesity among US adults, 1999–2000. The Journal of the American Medical Association, 288: 1723–27.233
21. Flegal K, Carroll M, Ogden C & Curtin L (2010). Prevalence and trends in obesity among US adults, 1999–2008. The Journal of the American Medical Association, 303: 235–41.
22. Ogden C & Carroll M (2010. Prevalence of obesity among children and adolescents: United States, trends 1964–1965 through 2007–2008. Centers for Diseases Control and Prevention. National Center for Health Statistics [Online]. Available: www.cdc.gov/nchs/data/hestat/
obesity_child_07_08/obesity_child_07_08.htm [Accessed 20 October 2011].
23. Wright J, Kennedy–Stephenson J, Wang C, McDowell M & Johnson C (2004). Trends in intake of energy and macronutrients – United States, 1971–2000. The Journal of the American Medical Association, 291: 1193–94.
24. Wright J & Wang C (2010). Trends in intake of energy and macronutrients in adults from 1999–2000 through 2007–2008. US Department of Health and Human Services. Centers for Disease Control and Pevention. NCHS Data Brief No. 49 [Online]. Available: www.cdc.gov/nchs/data/databriefs/db49.htm [Accessed 20 October 2011].
25. Stewart S, Cutler D & Rosen A (2009). Forecasting the effects of obesity and smoking on US life expectancy. New England Journal of Medicine, 361: 2252–60.
26. Peters A, Barendregt J, Willekens F, Mackenbach J, Al Mamun A & Bonneux L (2003). Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Annals of Internal Medicine, 238: 24–32.
27. Olshansky S, Passaro D, Hershow R, Layden J, Carnes B, Brody J, et al. (2005). A potential decline in life expectancy in the United States in the 21st century. New England Journal of Medicine, 352: 1138–45.
28. D’Arcy J. Holman C & Smith F (2008). Implications of the obesity epidemic for the life expectancy of Australians. Report to the Public Health Advocacy Institute of Western Australia [Online]. Available: www.phaiwa.org.au/index.php/publications-mainmenu-125/reports-mainmenu-127/61-obesity-and-life-expectancy [Accessed 20 October 2011].
29. Colagiuri S, Lee C, Colagiuri R, Magliano D, Shaw J, Zimmet P & Caterson I. (2010). The cost of overweight and obesity in Australia. Medical Journal of Australia, 192: 260–264.
30. Goss J (2008). Projection of Australian healthcare expenditure by disease, 2003 to 2033. Cat. No. HWE 43. Canberra: AIHW, (p21).
31. Finkelstein E, Trogdon J, Cohen J & Dietz W (2009). Annual medical spending attributable to obesity: payer- and service-specific estimates. Health Affairs – Web Exclusive, 28(5): w822–w831.
32. RAND Corporation (2007). Obesity and disability: the shape of things to come (RAND Health, Research Highlights), 2007 [Online]. Available: www.rand.org/pubs/research_briefs/2007/RAND_RB9043-1.pdf [Accessed 20 October 2011].
33. World Health Organization (2000). Obesity: preventing and managing the global epidemic. WHO Technical Report Series 894, Geneva: World Health Organisation.
34. Yusuf S, Hawken S, Ôunpuu S, Dans T, Avenzum A, Lanas F, et al. (2004). Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART Study): case-control study. The Lancet, 364: 937–52.234
35. Reeves M & Rafferty A (2005). Healthy lifestyle characteristics among adults in the United States, 2000. Archives of Internal Medicine, 165: 854–57.
36. Hopkins J (2005). Only 3% of US citizens follow good health advice. British Medical Journal, 330: 1044.
37. Atlantis E, Barnes E & Ball K (2007). Weight status and perception barriers to healthy physical activity and diet behavior. International Journal of Obesity, 32: 343–52.
38. Australian Broadcasting Corporation (2005). Transcript of Interview with the Hon. Tony Abbott MP. Four Corners. 17 October [Online]. Available: www.abc.net.au/4corners/content/2005/s1480656.htm [Accessed 20 October 2011].
39. Wakefield M, Loken B & Hornik R (2010). Use of mass media campaigns to change health behaviour. The Lancet, 376: 1261–71.
40. Johnson-Taylor W, Fisher R, Hubbard V, Starke-Reed P & Eggers P (2008). The change in weight perception of weight status among the overweight: comparison of NHANES III (1988–1994) and 1999–2004 NHANES. International Journal of Behavioral Nutrition and Physical Activity, 5: 9 [Online]. Available: www.ijbnpa.org/content/5/1/9 [Accessed 20 October 2011].
41. Johnson F, Cooke L, Croker H & Wardle J (2008). Changing perceptions of weight in Great Britain: comparison of two population surveys. British Medical Journal, 337: a494.
42. Giskes K & Siu J (2008). Do Australians perceive their weight status differentially and accurately? Implications for health promotion. Australian and New Zealand Journal of Public Health, 32: 183–84.
43. Bleich S (2008). Public perception of overweight. British Medical Journal, 337: 243–44 (p243).
44. Australian Institute of Health & Welfare (AIHW) (2004). Australia’s health 2004. Canberra: AIHW. Cat. No. AUS 44 (p122).
45. Australian Government (2011). Personally controlled electronic health record system: legislation issues paper [Online]. Accessed at: www.yourhealth.gov.au/internet/yourhealth/
publishing.nsf/Content/pcehr-legals [Accessed 21 October 2011].
46. Healthcare Identifiers Act 2010 (Cth).
47. Commonwealth of Australia (2009). Building the foundations for an e-health future: update on proposals for healthcare identifiers. Issued by the Australian Health Ministers’ Conference.
48. New York City, N.Y., Title24, Health Code §13.04.
49. New York City of Health and Mental Hygiene. The New YorkCity A1C Registry [Online]. Available: www.nyc.gov/html/doh/html/diabetes/diabetes-nycar.shtml [Accessed 21 October 2011].
50. Steinbrook R (2006). Facing the diabetes epidemic: mandatory reporting of glycosylated hemoglobin values in New York City. New England Journal of Medicine, 354: 545–48.
51. Mariner W (2007). Medicine and public health: crossing legal boundaries. Journal of Health Care Law & Policy, 10: 121–51.
52. Australian Institute of Health and Welfare (2006). Chronic diseases and associated risk factors in Australia, 2006. Canberra: AIHW. AIHW Cat. No. PHE 81.235
53. Tong B & Stevenson C (2007). Comorbidity of cardiovascular disease, diabetes and chronic kidney disease in Australia. Cardiovascular Disease Series no. 28. Cat. no. CVD 37. Canberra: AIHW.
54. Weiss C, Boyd C, Yu Q, Wolff J & Leff B (2007). Patterns of prevalent major chronic disease among older adults in the United States. Journal of the American Medical Association, 298: 1160–62.
55. Turrell G, Stanley L, de Looper M & Oldenburg B (2006). Health inequalities in Australia: morbidity, health behaviours, risk factors and health service use. Health Inequalities Monitoring Series No. 2. AIHW Cat. No. PHE 72. Canberra: Queensland University of Technology & AIHW.
56. King T, Kavanagh A, Jolley D, Turrell G & Drawford D (2006). Weight and place: a multilevel cross-sectional survey of area-level social disadvantage and overweight/obesity in Australia. International Journal of Obesity, 30: 281–87.
57. Kiim M, Berger D & Matte T (2006). Diabetes in New York City: public health burden and disparities. New York: New York City Department of Health and Mental Hygiene.
58. Medicare Benefits Schedule items 701, 703, 705, 707 [Online]. Available: www9.health.gov.au/mbs/search.cfm [Accessed 21 October 2011].
59. Australian Government (2010). Taking preventative action: a response to Australia: the healthiest country by 2020: the report of the National Preventative Health Taskforce [Online]. Available: www.preventativehealth.org.au/ [Accessed 21 October 2011].
60. Ashworth M & Jones R (2008). Pay for performance systems in general practice: experience in the United Kingdom. Medical Journal of Australia, 189: 60–61.
61. Scott A, Sivey P, Ait Ouakrim D, Willenberg L, Naccarella L, Furler J & Young D (2011). The effect of financial incentives on the quality of healthcare provided by primary care physicians. Cochrane Database of Systematic Reviews. Issue 9, Art. No.: CD008451.
62. Australian Government. Department of Health and Ageing. Practice Incentives Program [Online]. Available: www.medicareaustralia.gov.au/provider/incentives/pip/index.jsp [Accessed 21 October 2011].
63. Young D, Scott A & Best J (2010). For love or money? Changing the way GPs are paid to provide diabetes care. Medical Journal of Australia, 193: 67–68.
64. Australian Government. Department of Health and Ageing. Australian Primary Care Collaboratives Program (APCCP). [Online]. Available: www.health.gov.au/internet/main/publishing.nsf/Content/health-pcd-programs-apccp-index.htm [Accessed 21 October 2011].
65. Australian Primary Care Collaboratives (APCC). [Online]. Available: www.apcc.org.au/ [Accessed 21 October 2011].
66. Australian Government. Department of Health and Ageing (2010). Medicare Locals: discussion paper on governance and functions [Online]. Accessed at: www.yourhealth.gov.au/internet/yourhealth/publishing.nsf/content/MedicareLocalsDiscussionPaper [Accessed 21 October 2011].
67. National Preventative Health Taskforce. Australia: the healthiest country by 2020. The report of the National Preventative Health Strategy: the roadmap for action. 30 June 2009 [Online]. Accessed at: www.yourhealth.gov.au/internet/yourhealth/publishing.nsf/Content/nphs-report-roadmap [Accessed 21 October 2011].236
68. Balen A, Dresner M, Scott E & Drife J (2006). Should obese women with polycistic ovary syndrome receive treatment for infertility? British Medical Journal, 332: 434–35.
69. Peters M & Glantz L (2007). Should smokers be refused surgery? British Medical Journal, 334: 20–21.
70. Buyx A (2008). Personal responsibility for health as a rationing criterion: why we don’t like it and why maybe we should. Journal of Medical Ethics, 34: 871–74.
71. Onishi N (2008). Japan, seeking trim waists, measures millions. New York Times, 13 June 2008.
72. Thaler R & Sunstein C (2008). Nudge: improving decisions about health, wealth, and happiness. New Haven: Yale University Press.
73. Gostin L (2007). General justifications for public health regulation. Public Health, 121: 829–34.
74. Marteau T, Oliver A & Ashcroft R (2008). Changing behaviour through state intervention. British Medical Journal, 337: a2543.
75. Finkelstein E, Ruhm C & Kosa K (2005). Economic causes and consequences of obesity. Annual Review of Public Health, 26: 239–57.
76. James W (2007). The fundamental drivers of the obesity epidemic. Obesity Reviews, 9(Suppl. 1): 6–13.
77. Moodie R, Swinburn B, Richardson J & Somaini B (2006). Childhood obesity: a sign of commercial success, but a market failure. International Journal of Pediatric Obesity, 1(3): 133–38.
78. Jordan A & Robinson T (2008). Children, television viewing, and weight status: summary and recommendations from an expert panel meeting. Annals of the American Academy of Political and Social Science, 615: 119–32.
79. Rose G (1985). Sick individuals and sick populations. International Journal of Epidemiology, 14: 32–38 (p37).
80. Frank J, Lomax G, Baird P & Lock M (2006). Interactive role of genes and the environment. In J Heymann, C Hertzman, M Barer & R Evans (Eds). Healthier societies: from analysis to action (pp11–34). New York: Oxford University Press (p19).
81. World Health Organisation (2003). Diet, nutrition and the prevention of chronic diseases. World Health Organization Technical Report Series 916. Geneva, World Health Organization (pp54–71).
82. Kumanyika S (2007). Obesity prevention concepts and frameworks. In S Kumanyika & R Brownson (Eds). Handbook of obesity prevention (pp85–114). New York: Springer (p102).
83. Egger G & Swinburn B (1997). An ‘ecological’ approach to the obesity pandemic. British Medical Journal, 315: 477–80.
84. McKinlay J & Marceau L (2000). To boldly go … American Journal of Public Health, 90: 25–33 (pp28–29).
85. Sallis J, Cervero R, Ascher W, Henderson K, Kraft M & Kerr J (2006). An ecological approach to creating active living communities. Annual Review of Public Health, 27: 297–322.
86. Campbell I (2003). The obesity epidemic: can we turn the tide? Heart, 89(Suppl. II): ii22–ii24.237
87. Rose G (1981). Strategy of prevention: lessons from cardiovascular disease. British Medical Journal, 282: 1847–51.
88. Lang T & Rayner G (2007). Overcoming policy cacophony on obesity: an ecological public health framework for policymakers. Obesity Reviews, 8(Suppl. 1): 165–81.
89. Jain A (2005). Treating obesity in individuals and populations. British Medical Journal, 331: 1387–90.
90. Epstein R (2005). What (not) to do about obesity: a moderate Aristotelian answer. Georgetown Law Journal, 93: 1361–86.
91. Epstein R (2003). Let the shoemaker stick to his last: a defense of the ‘old’ public health. Perspectives in Biology and Medicine, 46(3): S138–59.
92. Sullum J (2004). The war on fat: is the size of your butt the government’s business? Reason, 8: 20–31.
93. Hall M (2003). The scope and limits of public health law. Perspectives in Biology and Medicine, 46(3): S199–S209.
94. Leeder S (2004). Ethics and public health. Internal Medicine Journal, 34: 435–39 (pp436–37).
95. Christakis N & Fowler J (2007). The spread of obesity in a large social network over 32 years. New England Journal of Medicine, 357: 370–79.
96. Jochelson K (2006). Nanny or steward? The role of government in public health. Public Health, 120: 1149–55.
97. Daube M, Stafford J & Bond L (2008). No need for nanny. Tobacco Control, 17: 426–26.
98. Hon. Tony Abbott MHR. Former Minister for Health and Ageing (Australia). Address to the Queensland Obesity Summit. 3 May 2006 [Online]. Accessed at: www.health.gov.au/internet/ministers/publishing.nsf/
Content/health-mediarel-yr2006-ta-abbsp030506.htm?OpenDocument&yr=2006&mth=5 [Accessed 21 October 2011].
99. Dorfman L & Wallack L (2007). Moving nutrition upstream: the case for reframing obesity. Journal of Nutrition Education and Behaviour, 39: S45–S50.
100. Warner K (2006). Tobacco policy research: insights and contributions to public health policy. In Warner K (Ed). Tobacco control policy (pp3–86). San Francisco: Jossey-Bass (p18).
101. Oliver T (2006). The politics of public health policy. Annual Review of Public Health, 27: 195–33.
102. Kersh R & Morone J (2002). The politics of obesity: seven steps to government action. Health Affairs, 21: 142–53.
103. Gostin L (2007). Law as a tool to facilitate healthier lifestyles and prevent obesity. Journal of the American Medical Association, 197: 87–90.
104. Magnusson R (2010). Obesity prevention and personal responsibility: the case of front-of-pack food labelling in Australia. BMC Public Health, 10: 662 [Online]. Available: www.biomedcentral.com/1471-2458/10/662 [Accessed 21 October 2011].
105. Roberto C, Schwartz M & Brownell K (2009). Rationale and evidence for menu-labeling legislation. American Journal of Preventive Medicine, 37: 546–51.238
106. Patient Protection and Affordable Care Act (US). H.R. 3590, §4205 (Nutrition Labeling of Standard Menu Items at Chain Restaurants and of Articles of Food Sold From Vending Machines).
107. Food Act 2003 (NSW). ss. 106K–106R.
108. McCarthy M (2004). The economics of obesity. The Lancet, 364: 2169–70.
109. Brownell K & Frieden T (2009). Ounces of prevention: the public policy case for taxes on sugared beverages. New England Journal of Medicine, 360: 1805–08.
110. Institute of Medicine (2009). Local government actions to prevent childhood obesity. Washington DC: The National Academies Press (pp4–11).
111. New York City Department of Health and Mental Hygiene. NYC Green Cart.[Online]. Available: www.nyc.gov/html/doh/html/cdp/cdp_pan_green_carts.shtml [Accessed 21 October 2011].
112. Tester J, Stevens S, Yen I & Laraia B (2010). An analysis of public health policy and legal issues relevant to mobile food vending. American Journal of Public Health, 100: 2038–46.
113. Coombes R (2011). Trans fats: chasing a global ban. British Medical Journal, 343: d5567.
114. Australian Institute of Health and Welfare (AIHW) (2010). Health expenditure Australia 2008–09. Health and Welfare Expenditure Series No. 425; Canberra: AIHW (pp8, 77).
115. World Health Organization (2004). Global strategy on diet, physical activity and health. WHA57.17.
116. National Obesity Prevention Act of 2008, H.R. 7179, 110th Congress, 2nd session, introduced into the House of Representatives, 27 September 2008 [Online]. Available: www.govtrack.us/congress/bill.xpd?bill=h110-7179 [Accessed 21 October 2011].
117. Patient Protection and Affordable Care Act (US). (P.L. 111–148), Title IV (§4001).
118. National Prevention Council (2011). National prevention strategy: America’s plan for better health and wellness. Rockville, Maryland: Office of the Surgeon General [Online]. Accessed at: www.healthcare.gov/centre/councils/nphpphc [Accessed 21 October 2011].
119. Department of Health (UK) (2003). Tackling health inequalities: a program for action (p37). [Online]. Available: www.dh.gov.uk/en/publicationsandstatistics/
publications/publicationspolicyandguidance/dh_4008268 [Accessed 21 October 2011].
120. Australian National Preventive Health Agency Act 2010 (Cth). s 11.
121. MacKay S, Antonopoulos N, Martin J & Swinburn B (2011). A comprehensive approach to protecting children from unhealthy food advertising and promotion. Obesity Policy Coalition; Melbourne [Online]. Available: www.opc.org.au/ [Accessed 21 October 2011].
122. Morley B, Chapman K, Mehta K, King L, Swinburn B & Wakefield M (2008). Parental awareness and attitudes about food advertising to children on Australian television. Australian and New Zealand Journal of Public Health, 32: 341–47.
123. Singh A, Mulder C, Twisk J, van Mechelen W & Chinapaw M (2008). Tracking of childhood overweight into adulthood: a systematic review of the literature. Obesity Reviews, 9: 474–88.
124. King L, Hebden L, Grunseit A, Kelly B, Chapman K & Venugopal K (2011). Industry self regulation 239of television food advertising: responsible or responsive? International Journal of Pediatric Obesity, 6: e390–98.
125. Kelly B, Chapman K, King L & Hebden L (2011). Trends in food advertising to children on free-to-air television in Australia. Australian and New Zealand Journal of Public Health, 35: 131–34.
126. Hebden L, King L, Chau J & Kelly B (2011). Food advertising on children’s popular subscription television channels in Australia. Australian and New Zealand Journal of Public Health, 35: 127–30.
127. Federal Trade Commission (2008). Marketing food to children and adolescents: a review of industry expenditures, activities, and self-regulation: a report to Congress. Federal Trade Commission.
128. Banks E, Jorm L, Rogers K, Clements M & Bauman A (2010). Screen-time, obesity, ageing and disability: findings from 91 266 participants in the 45 and up study. Public Health Nutrition, 14: 34–43.
129. Scully M, Dixon H & Wakefield M (2008). Association between commercial television exposure and fast-food consumption among adults. Public Health Nutrition, 12: 105–10.
130. Utter J, Scragg R & Schaaf D (2006). Associations between television viewing and consumption of commonly advertised foods among New Zealand children and young adolescents. Public Health Nutrition, 9: 606–12.
131. Wiecha J, Peterson K, Ludwig D, Kim J, Sobol A & Gortmaker S (2006). When children eat what they watch. Archives of Pediatric Adolescent Medicine, 160: 436–42.
132. Hesketh K, Wake M, Graham M & Waters E (2007). Stability of television viewing and electronic game/computer use in a prospective cohort study of Australian children: relationship with body mass index. International Journal of Behavioral Nutrition and Physical Activity, 4: 60 [Online]. Available: www.ijbnpa.org/content/4/1/60 [Accessed 21 October 2011].
133. Institute of Medicine (2006). Food marketing to children and youth: threat or opportunity. Washington DC: The National Academies Press.
134. Chou S, Rashad I & Grossman M (2008). Fast-food restaurant advertising on television and its influence on childhood obesity. Journal of Law and Economics, 51: 599–618 (p602).
135. Boyland E, Harrold J, Kirkham T, Corke C, Cuddy J, Evans D, et al. (2011). Food commercials increase preference for energy-dense foods, particularly in children who watch more television. Pediatrics, 128: e93–e100.
136. The Council of Better Business Bureaus. The Children’s Food and Beverage Initiative [Online]. Accessed at: www.bbb.org/us/about-children-food-beverage-advertising-initiative/ [Accessed 21 October 2011].
137. Harris J, Weinberg M, Schwartz M, Ross C, Ostroff J & Brownell K (2010). Trends in television food advertising: progress in reducing unhealthy marketing to young people? Yale University: Rudd Center for Food Policy & Obesity.
138. Harris J & Sarda V (2011). Trends in television food advertising to young people. 2010 Update. Yale University: Rudd Center for Food Policy & Obesity [Online]. Accessed at: www.yaleruddcenter.org/briefs.aspx [Accessed 21 October 2011].240
139. Kunkel D, McKinley C & Wright P (2009). The impact of industry self-regulation on the nutritional quality of foods advertised on television to children. Commissioned by Children Now [Online]. Available: www.childrennow.org/index.php/learn/
reports_and_research/article/576 [Accessed 21 October 2011].
140. Interagency Working Group on Food Marketed to Children (2011). Preliminary proposed nutrition principles to guide industry self-regulatory efforts: request for comments [Online]. Available: www.ftc.gov/opa/2011/04/foodmarket.shtm [Accessed 21 October 2011].
141. Mello M (2010). Federal Trade Commission regulation of food advertising to children: possibilities for a reinvigorated role. Journal of Health Politics, Policy and Law, 35: 227–76.
142. Kolish E (2011). The children’s food and beverage advertising initiative white paper on CFBAI’s Uniform Nutrition Criteria [Online]. Accessed at: www.bbb.org/us/children-food-beverage-advertising-initiative/info/ [Accessed 21 October 2011].
143. The Council of Better Business Bureaus (2011). Comments to the Interagency Working Group on food marketing to children [Online]. Accessed at: www.bbb.org/us/children-food-beverage-advertising-initiative/info/comments/ [Accessed 21 October 2011].
144. Australian Media and Communications Authority (2009). Children’s television standards 2009 [Online]. Available: www.acma.gov.au/WEB/STANDARD/pc=PC_310262 [Accessed 21 October 2011].
145. Jolly R (2011). Marketing obesity? Junk food, advertising and kids. Parliamentary Library Research Paper no. 9, 2010–11.
146. Broadcasting Services Act 1992 (Cth). s.122.
147. Kelly B & Chau J (2007). Children’s television sub-standards: a call for significant amendments. Medical Journal of Australia, 186: 18 (letter).
148. Chapman K, Nicholas P & Supramaniam R (2006). How much food advertising is there on Australian television? Health Promotion International, 21: 172–80.
149. Australian Communications and Media Authority (2009). Review of the children’s television standards, 2005: final report of the review. Canberra: ACMA [Online]. Accessed at: www.acma.gov.au/WEB/STANDARD/pc=PC_90095 [Accessed 21 October 2011].
150. Richard Ingleby, Lauren Prosser & Elizabeth Waters (2008). UNCROC and the prevention of childhood obesity: the right not to have food advertisements on television. Journal of Law and Medicine, 16: 49–56 (pp55–56).
151. Free TV Australia (2010). 2010 commercial television industry code of practice [Online]. Available: www.freetv.com.au/content_common/pg-code-of-practice.seo [Accessed 21 October 2011].
152. Broadcasting Services Act 1992 (Cth). s.123.
153. Australian Association of National Advertisers (2009). Code for advertising & marketing communications to children; August 2009 [Online]. Available: www.aana.com.au/codes.html [Accessed 21 October 2011].
154. MacKay S (2009). Food advertising and obesity in Australia: to what extent can self-regulation protect the interests of children? Monash University Law Review, 35: 118–46 (p134).241
155. Australian Food and Grocery Council (2009). The responsible children’s marketing initiative [Online]. Available: www.afgc.org.au/industry-codes/advertising-kids.html [Accessed 21 October 2011].
156. Hebden L, King L, Grunseit A, Kelly B & Chapman K (2011). Advertising of fast food to children on Australian television: the impact of industry self-regulation. Medical Journal of Australia, 195: 20–24.
157. Handsley E, Mehta K, Coveney J & Nehmy C (2009). Regulatory axes on food advertising to children on television. Australia and New Zealand Health Policy, 6: 1.
158. The UK Code of Broadcast Advertising (BCAP Code) (2010). [Online]. Accessed at: www.cap.org.uk/The-Codes/BCAP-Code.aspx [Accessed 21 October 2011].
159. The Contracting Out (Functions Relating to Broadcast Advertising) and Specification of Relevant Functions Order 2004 (UK). [Online]. Available: www.legislation.gov.uk/uksi/2004/
1975/pdfs/uksi_20041975_en.pdf [Accessed 13 December 2011].
160. Derbyshire D (2006). Ban all junk food ads before 9pm, says watchdog. The Telegraph (UK). 15 June [Online]. Available: www.telegraph.co.uk/news/uknews/1521313/Ban-all-junk-food-ads-before-9pm-says-watchdog.html [Accessed 21 October 2011].
161. Food Standards Agency (UK) (2009). Guide to using the nutrient profiling model [Online]. Available: food.gov.uk/healthiereating/advertisingtochildren/nutlab/nutprofmod [Accessed 21 October 2011].
162. Advertising Standards Authority (ASA). [Online]. Available: asa.org.uk/ [Accessed 21 October 2011].
163. Bond M, Williams M, Crammond B & Loff B (2010). Taxing junk food: applying the logic of the Henry Tax Review. Medical Journal of Australia, 193: 472–73.
164. Harper T & Mooney G (2010). Prevention before profits: a levy on food and alcohol advertising. Medical Journal of Australia, 192: 400–02.
165. Giang T, Karpyn A, Laurison H, Hillier A & Perry R (2008). Closing the grocery gap in underserved communities: the creation of the Pennsylvania Fresh Food Financing Initiative. Journal of Public Health Management Practice, 14: 272–79.
166. Commonwealth of Australia (2009). Australia’s future tax system – report to the Treasurer: part two, detailed analysis, volume 1 (The Henry Review) (pp320–22).
167. Mytton O, Gray A, Rayner M & Rutter H (2007). Could targeted food taxes improve health? Journal of Epidemiology and Community Health, 61: 689–94.
168. Goetzel R & Ozminkowski R (2008). The health and cost benefits of work site health-promotion programs. Annual Review of Public Health, 29: 303–23.
169. Baicker K, Cutler D & Song Z (2009). Workplace wellness programs can generate savings. Health Affairs, 29: 304–11.
170. World Economic Forum. Workplace Wellness and Chronic Disease Prevention [Online]. Available: members.weforum.org/en/initiatives/Wellness/index.htm. [Accessed 21 October 2011].242
171. World Economic Forum. Workplace Wellness Alliance [Online]. Available: www.weforum.org/issues/workplace-wellness-alliance. [Accessed 21 October 2011].
172. The Kaiser Family Foundation and Health Research & Educational Trust (2010). Employer health benefits 2010 annual survey [Online]. Available: ehbs.kff.org/ [Accessed 21 October 2011].
173. Patient Protection and Affordable Care Act (US). P.L. No. 111–148 (2009). s.10408.
174. Patient Protection and Affordable Care Act (US). P.L. No. 111–148 (2009). s.1001, inserting s. 2717 into the Public Health Service Act.
175. Patient Protection and Affordable Care Act (US). P.L. No. 111–148 (2009). s. 303.
176. 45 C.F.R. §146.121(b).
177. 45 C.F.R. §146.121(f).
178. Rothstein M & Harrell H (2009). Health risk reduction programs in employer-sponsored health plans: part II – law and ethics. Journal of Occupational and Environmental Medicine, 51: 951–57.
179. Patient Protection and Affordable Care Act (US). P.L. No. 111–148 (2009). s.1201, inserting s. 2705 into the Public Health Service Act.
180. Volpp K, Asch D, Galvin R & Loewenstein G (2011). Redesigning employee health incentives: lessons from behavioral economics. New England Journal of Medicine, 365: 388–90.
181. Jesson J (2008). Weighing the wellness programs: the legal implications of imposing personal responsibility obligations. Virginia Journal of Social Policy and the Law, 15: 217–98.
182. Patient Protection and Affordable Care Act (US). P.L. No. 111–148 (2009). s.1201, inserting ss.2702–03 into the Public Health Service Act.
183. Patient Protection and Affordable Care Act (US). P.L. No. 111–148 (2009). ss.1301–02.
184. The Healthy Workforce Act of 2009. S. 803/H.R. 1897 [Online]. Available: www.govtrack.us/congress/bill.xpd?bill=h111-1897 [Accessed 21 October 2011].
185. US Workplace Wellness Alliance [Online]. Available: www.uswwa.org/ [Accessed 21 October 2011].
186. Private Health Insurance Act 2007 (Cth). s. 55.5.
187. Council of Australian Governments (COAG) (2008). National partnership agreement on preventive health. Signed by Australian Governments. December [Online]. Available: www.anpha.gov.au/internet/anpha/
publishing.nsf/Content/publications [Accessed 21 October 2011].
188. National Partnership Agreement on Preventive Health: National implementation plan 2009–15, (pp38–48). [Online]. Available: www.anpha.gov.au/internet/anpha/
publishing.nsf/Content/publications [Accessed 21 October 2011].
189. NSW Health. Centre for Health Advancement (2010). NSW Healthy Workers Initiative: discussion paper. Centre for Health Advancement [Online]. Available: www.health.nsw.gov.au/Initiatives/healthyworkers/index.asp [Accessed 21 October 2011].243
190. Swinburn B, Sacks G, Hall K, McPherson K, Finegood D, Moodie M, et al. (2011). The global obesity pandemic: shaped by global drivers and local environments. The Lancet, 378: 804–14 (p807).
191. Yach D, Khan M, Bradley D, Hargrove R, Kehoe S & Mensah G (2010). The role and challenges of the food industry in addressing chronic disease. Globalization and Health, 6: 10 [Online]. Available: www.globalizationandhealth.com/content/6/1/10 [Accessed 21 October 2011].
192. Stolberg S (2011). Wal-Mart shifts strategy to promote healthy foods. New York Times, 20 January 2011.
193. Food Standards Australia New Zealand (FSANZ). Food standards code [Online]. Available: http://www.foodstandards.gov.au/code/Pages/default.aspx [Accessed 21 October 2011].
194. Walker K, Woods J, Rickard C & Wong C (2007). Product variety in Australian snacks and drinks: how can the consumer make a healthy choice? Public Health Nutrition, 11: 1046–53.
195. New York City, Department of Health and Mental Hygiene. Board of health approves regulation to phase out artificial trans fat [Online]. Available: www.nyc.gov/html/doh/html/cardio/cardio-transfat-healthcode.shtml [Accessed 21 October 2011].
196. Mello M (2009). New York City’s war on fat. New England Journal of Medicine, 360: 2015–20.
197. Brown I, Tzoulaki I, Candeias V & Elliott P (2009). Salt intakes around the world: implications for public health. International Journal of Epidemiology, 38: 791–813 (p807).
198. He F & MacGregor G (2009). A comprehensive review of salt and health and current experience of worldwide salt reduction programmes. Journal of Human Hypertension, 23: 363–84.
199. He F & MacGregor G (2010). Reducing population salt intake worldwide: from evidence to implementation. Progress in Cardiovascular Diseases, 52: 363–82.
200. Cappuccio F, Capewell S, Lincoln P & McPherson K (2011). Policy options to reduce population salt intake. British Medical Journal, 343: d4995.
201. Australian Government. Department of Health and Ageing. Food and health dialogue [Online]. Available: www.foodhealthdialogue.gov.au/internet/
foodandhealth/publishing.nsf/Content/Home [Accessed 24 October 2011].
202. He F, Marrero N & MacGregor G (2008). Salt intake is related to soft drink consumption in children and adolescents: a link to obesity? Hypertension, 51: 629–34.
203. Food Standards Agency (UK) (2009). Salt reduction targets. 18 May [Online]. Accessed at: www.food.gov.uk/scotland/scotnut/salt/saltreduction [Accessed 24 October 2011].
204. New York City. Department of Health and Mental Hygiene. Cutting salt, improving health [Online]. Available: www.nyc.gov/html/doh/html/cardio/cardio-salt-initiative.shtml [Accessed 24 October 2011].
205. Forshee R (2008). Innovative regulatory approaches to reduce sodium consumption: could a cap-and-trade system work? Nutrition Reviews, 66: 280–85.
206. Sugarman S (2009). Salt, high blood pressure, and performance-based regulation. Regulation & Governance, 3: 84–102.244
207. Institute of Medicine (IOM) (2010). Strategies to reduce sodium intake in the United States. Washington, DC: The National Academies Press (pp8–15ff).
208. Australian National Preventive Health Agency Act 2010 (Cth). s. 11.
209. Food Standards Australia New Zealand Act 1991 (Cth). s. 17.
210. Malone R (2010). The tobacco industry. In W Wiist (Ed). The bottom line or public health: tactics corporations use to influence health and health policy, and what we can do to counter them (pp155–91). New York: Oxford University Press.
211. World Health Organization (2008). Guidelines for implementation of Article 5.3 of the WHO Framework Convention on Tobacco Control – on the protection of public health policies with respect to tobacco control from commercial and other vested interests of the tobacco industry. Decision FCTC/COP3(7). November.
212. Roberts I (2008). Corporate capture and Coca-Cola. The Lancet, 372: 1934–35.
213. Chopra M & Darnton-Hill I (2004). Tobacco and obesity epidemics: so different after all? British Medical Journal, 328: 1558–60
214. Ludwig D & Nestle M (2008). Can the food industry play a constructive role in the obesity epidemic? Journal of the American Medical Association, 300: 1808–11.
215. Yach D (2008). Food companies and nutrition for better health. Public Health Nutrition, 11: 109–11.
1 Sydney Law School, University of Sydney.
2 The term ‘burden of disease’ refers to a combination of years of life lost through premature mortality, combined with the years of healthy life lost, due to disease. Typically, the burden of disease is measured in disability-adjusted life years, or DALYs.
3 Following a pilot project in the Bronx, patients in New York City with blood glucose levels above a certain level receive information (on an opt-out basis) about the lifestyle changes required to reduce health risks. Treating physicians are given a report which enables them to identify patients whose diabetes is not well controlled, and a summary of glycaemic control among patients in the practice which can be compared with a NYC benchmark.
4 For patients with diagnosed chronic or complex health conditions, Medicare rebates are payable for a limited number of consultations with allied health professional services, as part of an Enhanced Primary Care plan coordinated by a general practitioner: Australian Government Department of Health and Ageing. Enhanced Primary Care Program, at: www.health.gov.au/epc.
5 As Marteau, Oliver and Ashcroft [74] point out, ‘Unfortunately, the health costs of many behaviours occur in the future, whereas their benefits are enjoyed in the present. The so-called obesogenic environment reflects the operation of these two principles – that is, an environment that contains a plethora of readily realized options that offer immediate gratification but that cause and sustain obesity’.
6 As Joseph Sullum (90) writes, ‘The war on fat … reflects an anti-capitalist perspective that views people as helpless automatons manipulated into consuming whatever big corporations choose to produce. The anti-fat crusaders want to manipulate us too, but for our own good’ (p23).
7 Examples of portfolio agencies, each with their establishing acts, include the National Health and Medical Research Council (NHMRC), Cancer Australia, and the National Blood Authority (NBA).