14
Whole of society approaches to preventing obesity and diabetes
The current diabetes and obesity epidemic is largely a societally and environmentally constructed health problem. Physical inactivity and excessive intake of nutrient-poor and energy-dense foods are the two most important proximal behavioural contributors to the unprecedented diabetes and obesity levels currently facing many nations. Traditionally, individual behaviour change approaches and counselling, often combined with judicious use of evidence-based pharmacological agents, have been the mainstay of efforts to reduce these health risks. A newer socio-ecological approach refocuses solutions on tackling broader environmental causes of obesity and type 2 diabetes. This chapter examines promising societal and environmental responses that enable and support regular physical activity and healthy eating across populations. These approaches include redesigning the built environment, providing active transport options, promoting the availability and accessibility of healthy food choices, restricting promotion of unhealthy foods, and implementing ongoing social marketing strategies to influence sustained healthy eating and physical activity behaviours. Implications for policy development and how public health can work with various sectors of society to halt the rise in obesity and diabetes are discussed.
If it takes a village to raise a child, it takes the organised efforts of a society to ensure that all of its children grow up to be healthy. A public health approach, by definition, involves ‘the science and art of preventing disease, prolonging life and promoting health through the organized efforts and informed choices of society, organizations, public and private, communities and individuals’ [1].
Diabetes mellitus, in its commonest form known as type 2 diabetes, and obesity, share some of the same modifiable risk factors, such as low physical activity, prolonged sitting, and too much energy-dense, nutrient-poor foods. As a society, we have created a social and physical environment that facilitates being sedentary and encourages excessive food consumption. High-kilojoule convenience foods are readily available and more affordable than fresh food, and heavily marketed to all ages. We have designed transport systems to minimise physical effort, and prioritised private motor vehicles over public transport by building motorways instead of railways or rapid bus transit corridors. Unchecked development on urban fringes
246creates a vast suburban sprawl, making distances too great for walking and cycling. These structural problems facilitate and reinforce individual behaviours, with inactive options logistically easier, and unhealthy food choices cheaper and more accessible. This chapter examines the way this has occurred, and suggests ways to reorganise the efforts of society to create a healthier physical and social environment.
A socio-ecological perspective as a societal solution to preventing obesity and diabetes
Until recently, most obesity and diabetes prevention strategies have involved behaviour change programs that focus on the biology and psychology of the individual. This approach has some limitations. First, even optimal interventions that persuade individuals to eat better and be more physically active tend to have either weak or short-lived effects [2, 3]. This, together with the rapid rise in obesity and diabetes globally over the past three decades [4], suggests that the causes of obesity and diabetes are beyond individual biology and psychology. Second, individual and education-based programs tend to have low population reach, and usually enrol motivated individuals or those with already high levels of risk. While this strategy yields great effects for high-risk individuals, it has minimal effects on population levels of obesity and diabetes because it does not reach the largest numbers of people, those who are at average risk. As the causes of obesity and diabetes are likely to be linked to broader environmental and societal changes [5, 6, 7] that can impact populations, there is a need for a shift in thinking and solutions to these problems.
To achieve large and sustained public health gains through the prevention of diabetes and obesity, the whole population needs to be targeted regardless of their current health status. Even small shifts in the average level of a risk factor within a population would result in large population effects overall [8]. Optimal public health strategies then would encourage everyone in the community to make small shifts in lifestyle habits every day [9].
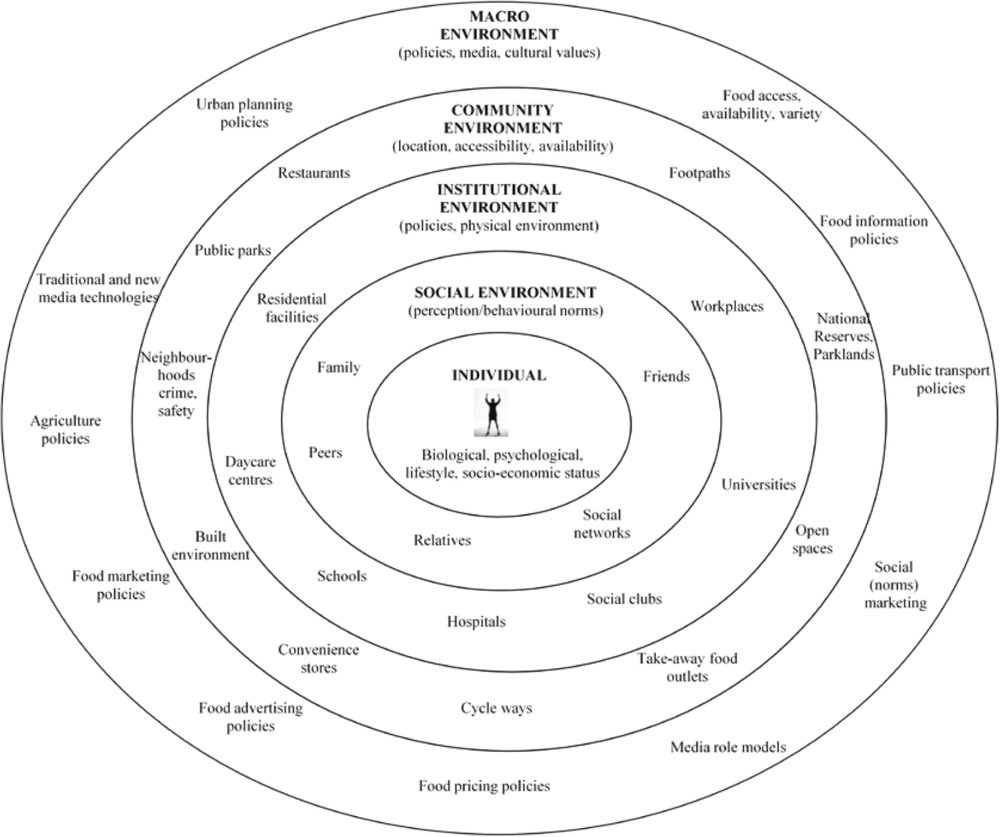
Socio-ecological perspectives describe the multilevel influences on individual health behaviour [10, 11]. Figure 1 shows these influences, conceptually drawn as concentric circles of influences from proximal to distal. Individual characteristics, beliefs and attitudes comprise the inner circle, surrounded by immediate influences of friends and family. Institutional environmental influences then come into play, such as the food environment and physical environment at workplaces, schools and places where people spend most of their time. Broader outer circles reflect the urban community environment, and the economic and cultural environments in which people live; these can influence social norms, food production and availability, public open space provision, and the existence of active transport options in communities and cities.
The socio-ecological perspective posits that prevention programs and policies that change people’s knowledge, attitudes and skills without changing the societal and physical environments in which people work, live and play, are unlikely to be effective. Prevention strategies must operate on multiple levels, including individually targeted and tailored behaviour change components, as well as environment and social support strategies to make it easier for individuals to adopt healthy practices. Becoming more physically active is 247easier where there are safe walking/cycling paths in the neighbourhood, exercise stations or quality playgrounds in local parks. Healthy food choices are facilitated by neighbourhood shops that stock affordable and nutritious food. Interventions that cultivate social norms about the benefits of physical activity and healthy eating, policies that ensure physical activity programs are available in parks, or initiatives that emphasise the provision of comprehensible nutrition information at point of purchase all have potential important benefits. The following sections examine some promising societal and environmental responses that facilitate regular physical activity and healthy eating across populations.
Physical activity environments
Redesigning the built environment for walking and cycling
Over half the Australian population is not reaching minimal recommendations of around 150 minutes per week (2.5 hours) of moderate–vigorous physical activity for health benefits [12]. This equates to approximately half an hour of activity accumulated over at least five separate sessions on most days each week. The target amount of 150 minutes per week 248can also be accrued in short bouts of ten minutes or more. Recommendations for weight maintenance or weight loss are substantially greater, typically around 60 to 90 minutes daily [13].
A key contributor to decreased daily physical is increased reliance on motor vehicles. Over 75% of Australians live in an urban setting [14], with a third of all car trips under three kilometres and a half under five kilometres, distances that could easily be walked or cycled. Short trips by bicycle can in fact be faster in an inner city context than driving [15]. If available, public transport as an alternative to driving can also provide some physical activity. Catching a bus or train generally involves a walk at either end of the trip. Walking, cycling or using public transport is often called ‘active travel’.
Cycling is an important form of active travel. However, while about 10% of Australians will cycle in any given year, only 1%–2% cycle daily [16]. The opportunity to cycle depends on good cycling infrastructure, with a network of well-connected bicycle lanes and routes. This is particularly needed to overcome the perception of the dangers of cycling, ideally by separating cyclists from mainstream car traffic [17]. Recent cycling infrastructure development in central Sydney that applied these guidelines has resulted in an increase in the observed numbers of daily bicycle trips [18].
It is also important to encourage walking as a form of active travel. Walking accounts for two-thirds of women’s and one-half of men’s health enhancing physical activity [19], yet, the built environment in urban areas discourages walking. More sustained walking and cycling behaviours can be encouraged by urban design that creates a physical environment more conducive to cycling and walking. For example, occasional or non-regular riders do not ride long distances for utilitarian purposes. One way to reduce trip distances is to develop cities with higher density and greater mixed land use (having residential zoning near commercial areas). Urban planners and transport engineers could create more walkable physical environments through medium-density housing, connection of street networks and having mixed-use destinations (having local shops, businesses and residential dwellings in the same neighbourhood) [20]. This means more people can live near where they work, removing the need to commute long distances. Most people will choose the easiest, cheapest and most convenient way to get to work. If pedestrian and cycling footpaths were available, active transport is more likely.
While there is some truth in the idea of ‘build it and they will come’, the optimal approach is for good cycling and walking infrastructure to be built and promoted to the public and prospective users. A community-based project in Western Sydney to encourage cycling and the use of existing bicycle paths found a significant increase as a result of social marketing and behavioural programs [21, 22]. Similarly, there is a need to create and then promote walkable environments to the community, and change community perceptions around walking as a mode of transport.249
Redesigning public spaces for active living and recreational activities
Active living refers to opportunities for people to incorporate active travel and recreational activities into their everyday lives. Town and city residents rely on public spaces such as natural reserves and public parks as venues for outdoor recreational activities [23]. Theoretically, public spaces are more likely to be used by the general population than indoor sport and exercise facilities such as the gym [24]. Epidemiological evidence shows that people living in activity-friendly environments with green spaces, playgrounds and walking/jogging paths tend to be more physically active [25, 26, 27, 28], and both adults and children have reduced obesity risk [29, 30]. A recent systematic review found open space preservation to be associated with increased physical activity levels, primarily walking [31]. Yet, public spaces such as neighbourhood parks are an underutilised environmental setting for promoting physical activity. This reflects a research area in evolution, with much research describing associations between park characteristics and physical activity [27]. Limited evidence notwithstanding, the evidence to date supports the notion of neighbourhood parks as a promising environmental setting for promoting recreational activities. Since public spaces are amenable to change, improving their conduciveness to physical activity has good potential to improve the quality of community life [32].
Two ‘naturalistic’ studies in Sydney evaluated the impact of park improvements on physical activity levels. One study in Western Sydney did not reach conclusive findings about the impact of improving the environment in three parks on physical activity participation [33]. Another study in an inner Sydney suburb found improving children’s playgrounds increased usage [34]. Despite their potential policy implications, intervention evidence from these naturalistic studies, so called because they aimed to evaluate the effectiveness of environmental changes opportunistically, remains limited [35, 36].
Even though improving facilities and amenities is an important step, the socio-ecological perspective would propose that an integrated approach would comprise promotion to increase awareness, and organised activity programs in renovated public spaces are also needed to motivate community use [35, 37]. Local councils and governments are in the position to define public space (re)design for supporting community-wide physical activity participation, and ensure that appropriate recreational programs are provided and promoted to the community.
Narrowing the health inequality gap through environmental strategies
Health inequalities between neighbourhoods have been well documented in Australia [38]. People living in socioeconomically disadvantaged areas have higher rates of chronic diseases and lower leisure-time physical activity than those in more affluent neighbourhoods [39]. One benefit of a socio-ecological perspective in a comprehensive multilevel prevention obesity/diabetes program is that the interventions can impact whole populations, not just motivated individuals who attend clinics or specific programs. Based on this perspective, the development of public infrastructure could contribute to reducing the differences in health behaviours between poor and wealthy areas [40, 41, 42, 43].250
Positive relationships between access to quality public spaces and increased physical activity and reduced obesity risk are most apparent among residents living in socioeconomically disadvantaged areas, the elderly and homemakers [27, 30]. This suggests that improving the quality of public spaces (eg access, aesthetics, functionality, proximity, perceived safety), may counter the effects of neighbourhood socioeconomic disadvantage, and contribute to narrowing the diabetes and obesity inequality gap between areas [44].
Summary of physical activity environments
Living in activity-friendly communities can facilitate active transport and recreation for every person regardless of their socioeconomic status. Although more evidence is needed to demonstrate direct links between specific environmental infrastructure and physical activity, public health experts consider the evidence sufficient to recommend policy interventions to reshape approaches to urban planning and built environment designs for supporting active living [45]. Increasing incidental and everyday physical activities through environmental approaches may contribute sufficiently to increase total energy expenditure, and to have a role in obesity and diabetes prevention.
Food environments
Despite living in a society that has a plentiful supply of nutritious foods, the majority of Australian adults and children do not eat in accordance with dietary guidelines, and in particular consume excessive amounts of energy-dense, nutrient-poor (EDNP) foods. Energy-dense, nutrient-poor foods refer to foods high in total energy, fat and/or sugar and with little positive nutritional value. Examples include many fast foods, fried foods, fatty meats, cakes, confectionery and sweetened drinks.
Population increases in the prevalence in overweight and obesity indicate that a significant proportion of adults and children consume more energy than they require on a regular basis. In 2007, EDNP foods contributed to 35% of the daily energy intake of children aged two to 16 years, which is twice the recommended limit of 5%–20% [46]. For adults, EDNP comprised 36% of energy intake in 1995 [47].
As with physical activity, the science of nutrition education started with programs and clinicians providing advice to individuals. The approach has broadened to encompass the food environment, social norms and broader environmental influences, as highlighted by the socio-ecological framework. Food consumption patterns reflect the interactions between individual factors, such as food preferences and disposable income, and environmental factors, such as food availability, price and marketing. Despite the positive aspects of our food supply, our food environment in fact promotes excessive food consumption, particularly of EDNP foods. Energy-dense, nutrient-poor foods are widely available and extensively marketed, through multiple media as well as at point of sale [48]. These environmental influences are particularly strong, as nutrition information about specific food products is not highly accessible at point of sale. As such, there are many barriers to ‘making healthy choices easier choices’.251
Redesigning environments to improve the availability of healthy foods
People’s access to healthy foods is influenced by the availability of healthy foods in their neighbourhood, or their access to transport to travel to more distant food retail outlets. A landmark study of 221 census areas with over 10 000 residents in the US found that residents increased their fruit and vegetable consumption by 32% for each additional supermarket in their census area [49]. Further studies in both Australia and other developed countries have consistently found that supermarkets offer a predictably large range of healthier food items and at lowest costs [50, 51].
Much of the work exploring food environments has focused on access differentials between more and less socioeconomically advantaged areas as a possible explanation of social gradients in the prevalence of obesity. This corresponds to the concept of ‘deprivation amplification’, where disadvantages arising from poorer quality environments amplify individual disadvantages in ways that are detrimental to health [52].
Some international studies have described reduced food availability and quality, and increased price of healthier foods in more disadvantaged neighbourhoods and rural areas [53, 54]. However, this has not been a consistent finding, and healthy food availability probably also depends on other factors such as population density and urban planning.
Two studies from the UK prospectively examined the impact of introducing a supermarket into an area which did not previously have one. Whilst one study found a substantial increase in nearby residents’ consumption of fruit and vegetables [55], the other only found a change in those residents who switched to do all their shopping at the new supermarket [56]. A US study which followed 5115 people in several cities for 15 years, found that easy access to fresh food stores did not improve food choices [57]. The study also found that living near fast-food outlets was associated with increased consumption of fast food. Thus, limiting the availability and access to fast foods may be as important as increasing the availability and access of healthy food.
Altogether, the body of research on community food availability reinforces the public health value of mixed land use, with convenient location of supermarkets, and public transport routes, active transport infrastructure and community transport options to ensure people have good access to supermarket destinations [58].
Redesigning the nutrition information environment: food and menu labelling
People’s access to healthy foods is also influenced by their ability to identify healthier food products. Thus, nutrition information systems are considered by public health professionals as important communication tools to inform and potentially influence consumers. They are also of interest to the food industry as promotional and marketing tools which offer opportunities for communicating both factually and persuasively.
Recently, front-of-pack (FOP) signposting schemes have been proposed as a consumer-friendly tool to assist consumers in making at-a-glance decisions about a product’s nutritional composition [59]. The value of a FOP system has been clearly identified, 252and research indicates that shoppers achieve higher accuracy in determining product healthiness with simpler nutritional formats, particularly traffic light systems [60]. However, the public health and food industry interests in nutritional labelling have led to a plethora of FOP labelling systems over recent years, and there is now evidence that the simultaneous operation of multiple systems creates confusion and lack of trust in such information [61]. The need to have a single, consistent system in operation provides a strong argument for a mandatory labelling system. Researchers have also shown that the use of uniform FOP labelling may have indirect impacts on food supply, and may influence reformulation or development of healthier products [62].
As Australians are increasingly purchasing and relying on foods prepared outside the home, there has also been increased research and policy emphasis on the provision of nutrition information at point of purchase in food service outlets, despite inconclusive evidence regarding the effects of such labelling on purchasing and consumption [63]. In the interests of consumer information, the New South Wales (NSW) government has introduced legislation requiring all chain restaurants with 20 or more locations in NSW or 50 or more locations nationally to include kilojoule labelling on their menu boards for all ‘standard menu items’ from 2012. This follows the introduction of state menu nutrition labelling policies across the US since 2003, and a national bill in March 2010.
Redesigning the nutrition information environment: limiting food marketing
Whilst public health seeks to provide consumers with nutrition information, food marketing is designed to persuade consumers to buy specific food products, and tends to undermine public health nutrition efforts. The specific concern arises as food marketing is highly pervasive and the majority of foods advertised are EDNP [46].
Australian and international studies indicate that reductions in advertising of unhealthy foods and beverages are likely to be a cost-effective (and probably cost-saving) strategy for obesity prevention and chronic disease prevention [64, 65].
Many governments and international agencies have concerns about the marketing of foods and non-alcoholic drinks to children. In May 2010 the World Health Organization stipulated that governments should develop appropriate policies and set clear definitions for key components of restrictions on marketing of foods and drinks to children [66]. On the basis of the evidence, the Australian Government’s National Preventative Health Task Force (2009) recommended government restrictions to reduce children’s exposure to advertising of unhealthy foods [67]. In response, the Australian Government decided it would monitor the impact of self-regulation on ‘reducing children’s exposure to advertising of energy-dense, nutrient-poor foods and beverages’, before any further government action [68].
Since then, studies indicate that industry self-regulation remains inadequate in reducing Australian children’s exposure to junk food advertising on television, and children still see the same amount of television advertising for unhealthy foods as they did before industry self-regulation was introduced in 2009 [69, 70]. The lack of impact partially reflects the 253voluntary participation and lenient specifications of the industry self-regulatory standards [71]. For example, food companies were found to consistently stipulate higher thresholds for negative nutrients (saturated fats, added sodium and sugars) compared with existing professional criteria [72].
The rationale for government action to limit food marketing to children is gaining momentum. Only government is in the position to set a framework of advertising standards defining the types of foods and drinks deemed appropriate for advertising to children based on a food or drink’s nutrient profile, and assessed using a standardised, independent nutrient-profiling tool; and ensure that these standards apply to all food companies.
Summary of food environments
Redesigning food environments to make them more conducive to healthy eating is fundamental to promoting nutrition at a population level. Individuals need to be informed about healthy food options, but the broader environment that promotes, advertises and creates accessible food purchasing also need to be influenced, if population dietary patterns are to be changed. Policies can ensure that healthy foods are widely available and accessible, that people have easy access to accurate nutritional information in order to identify healthier foods, and that this information is not undermined by persuasive marketing. These actions can contribute to a comprehensive approach to public health nutrition and obesity prevention.
Creating societal norms for active living and healthy eating
Even environmental and policy changes may not be sufficient to motivate people to become physically active or eat healthily. Cultural values and social norms also play a key role in the types and quantities of food and drinks consumed; and how much and where physical activity is incorporated into daily living. When individuals engage in active modes of travel, some may do so because they see others doing it, and consider such behaviour the norm in their society. Accordingly, striving for healthy eating habits and regular physical activity can be more difficult if such practices are not valued or perceived to be desirable within a society.
In this context, social marketing is well placed to augment the benefits of environmental and policy changes in ways that are consistent with a socio-ecological framework [67, 73]. Geoffrey Rose reminded us that ‘It makes little sense to expect individuals to behave differently from their peers; it is more appropriate to seek a general change in behavioural norms and in the circumstances which facilitate their adoption’ [74]. Diverse and complementary chronic disease prevention initiatives therefore must be supported by consistent messages to reshape cultural values and social norms. This includes promoting practical, simple everyday changes in lifestyles [75], as well as cultivating political and social movements for active communities and a healthy food supply. In this situation, social marketing to change social norms has an advocacy component, including targeting key decision-makers about a policy development or resource allocation decision [76]. This strategy has been widely used in tobacco control, where there is already strong community 254support for tobacco control legislation. In obesity and diabetes prevention, the goal is to replace the ‘obesogenic’ features of environment with environments that make it easier for individuals to be active and make healthy nutrition choices.
Preventing obesity and type 2 diabetes is a shared responsibility
The socio-ecological approach provides a framework to implement a broad range of environmental and policy initiatives across multiple levels of society. This involves directing physical activity and nutrition initiatives at infrastructure (eg active living communities), institutions (eg retail settings, workplaces), policies and regulations (eg food marketing to children), media (eg coverage of health issues), and social norms (eg relationships, behaviours). Building footpaths and regulating availability of fast food outlets are more permanent strategies, and can impact larger numbers of people than individual-based health education programs that target smaller numbers of motivated individuals with high risks. Making these changes at the whole population level is a necessary antecedent to diabetes prevention and to weight maintenance and obesity prevention.
The reality of widespread societal and environmental initiatives will require committed and sustained advocacy and resources, with positive population-wide changes in obesity and diabetes taking several years to manifest. Acknowledging this complexity, solving the obesity and diabetes ‘epidemics’ will require building multidisciplinary collaborations between scientists and policy-makers. Strengthening the research translation pathways, from findings to practice and policy enactment will be an important component of such collaborations. It is important to recognise that all tiers of government and various sectors of society shape beliefs and practices about physical activity and eating. As such, all are responsible for society’s health. Organised public health efforts involve collaborations across government sectors and with different groups in society, such as industry, consumer groups, civil society and the media. As the City of Sydney has shown, urban renewal for active living across the life span and for all sub-population groups is possible in Australia. Government leadership, social planning and urban renewal that engages communities, businesses and relevant stakeholders is fundamental to the process. Only then will a society be able to hardwire regular physical activity and healthy eating into its everyday fabric and ensure more sustainable healthy behaviours to prevent obesity, diabetes and other chronic diseases.
References
1. Winslow CE (1920). The untilled fields of public health. Science, 51(1306): 23–33.
2. Centers for Disease Control and Prevention (CDC) (2010). Guide to community preventive services: promoting good nutrition [Online]. Available: www.thecommunityguide.org/nutrition/index.html [Accessed 23 July 2011].
3. Foster C, Hillsdon M & Thorogood M (2005). Interventions for promoting physical activity. Chichester, UK: John Wiley & Sons, Ltd.255
4. World Health Organization (2005). Preventing chronic disease: a vital investment. WHO global report. Geneva: World Health Organization.
5. Bauman A, Ma G, Cuevas F, Omar Z, Waqanivalu T, Phongsavan P, Keke K & Bhushan A (2011). Cross-national comparisons of socioeconomic differences in the prevalence of leisure-time and occupational physical activity, and active commuting in six Asia-Pacific countries. Journal of Epidemiology and Community Health, 65(1): 35–43.
6. Suhrcke M, Nugent RA, Stuckler D & Rocco L (2006). Chronic disease: an economic perspective. London: Oxford Health Alliance.
7. Trinh OTH, Nguyen ND, Phongsavan P, Dibley MJ & Bauman AE (2009). Prevalence and risk factors with overweight and obesity among Vietnamese adults: Caucasian and Asian cut-offs. Asia Pacific Journal of Clinical Nutrition, 18(2): 226–33.
8. Rose G (2001). Sick individuals and sick populations. International Journal of Epidemiology, 30(3): 427–32.
9. World Health Organization (2004). Global strategy on diet, physical activity and health. Geneva: World Health Organization.
10. McLeroy KR, Bibeau D, Steckler A & Glanz K (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4): 351–77.
11. Stokols D (1992). Establishing and maintaining healthy environments: toward a social ecology of health promotion. American Psychologist, 47(1): 6–22.
12. Australian Institute of Health and Welfare (2010). Australia’s health 2010. Australia’s health series no. 12. Sydney: AIHW.
13. Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD & Bauman A (2007). Physical activity and public health: updated recommendations for adults from the American College of Sports Medicine and the American Heart Association. Medicine & Science in Sports Exercise, 39(8): 1423–34.
14. Australian Government (2010). Our cities: building a productive, sustainable and liveable future. Discussion paper. Sydney: Infrastructure Australia.
15. Australian Bicycle Council (2010). The Australian national cycling strategy 2011–2016. Sydney: Austroads.
16. Merom D, van der Ploeg HP, Corpuz G & Bauman AE (2010). Public health perspectives on household travel surveys active travel between 1997 and 2007. American Journal of Preventive Medicine, 39(2): 113–21.
17. Daley M, Rissel C & Lloyd B (2007). All dressed up and no-where to go? A qualitative research study of the barriers and enablers to cycling in inner Sydney. Road and Transport Research, 16: 42–52.
18. City of Sydney (2011). Bike riding booms around Sydney’s new cycleways. Sydney: City of Sydney.
19. Merom D, Bauman A & Ford I (2004). The public health usefulness of the exercise recreation and sport survey (ERASS) surveillance system. Journal of Science and Medicine in Sport, 7(1): 32–37.256
20. Bauman AE & Bull FC (2007). Environmental correlates of physical activity and walking in adults and children: a review of reviews. London: National Institute of Health and Clinical Excellence [Online]. Available: www.nice.org.uk [Accessed 14 June 2011].
21. Bauman A, Rissel C, Garrard J, Kerr I, Speidel R & Fishman E (2008). Cycling: getting Australia moving. Barriers, facilitators and interventions to get more Australians physically active through cycling. Melbourne: Cycling Promotion Fund.
22. Rissel C, New C, Wen LM, Merom D, Bauman AE & Garrard J (2010). The effectiveness of community-based cycling promotion: findings from the Cycling Connecting Communities project in Sydney, Australia. International Journal of Behavioral Nutrition and Physical Activity, 7(1): 8.
23. Sydney Urban Parks Education and Research Group (2002). Research report: Sydneysiders’ use of parks and gardens, 2001. Sydney: Centre for Visitor Studies.
24. Bendimo-Rung AL, Mowen AJ & Cohen DA (2005). The significance of parks to physical activity and public health: a conceptual model. American Journal of Preventive Medicine, 28: 159–68.
25. Brownson RC, Baker EA, Housemann RA, Brennan LK & Bacak SJ (2001). Environmental and policy determinants of physical activity in the United States. American Journal of Public Health, 91(12): 1995–2003.
26. Davidson KK & Lawson C (2006). Do attributes of the physical environment influence children’s level of physical activity? International Journal of Behavioral Nutrition and Physical Activity, 3(19): 1–17.
27. Kaczynski AT & Henderson KA (2007). Environmental correlates of physical activity: a review of evidence about parks and recreation. Leisure Sciences, 29: 315–54.
28. Owen N, Humpel N, Leslie E, Bauman A & Sallis JF (2004). Understanding environmental influences on walking: review and research agenda. American Journal of Preventive Medicine, 27(1): 67–76.
29. Bell JF, Wilson JS & Liu GC (2008). Neighborhood greenness and 2-year changes in body mass index of children and youth. American Journal of Preventive Medicine, 35(6): 547–53.
30. Nielson TS & Hansen KB (2007). Do green areas affect health? Results from a Danish survey on the use of green areas and health indicators. Health & Place, 13: 839–50.
31. Durand CP, Andalib M, Dunton GF, Wolch J & Pentz MA (2011). A systematic review of built environment factors related to physical activity and obesity risk: implications for smart growth urban planning. Obesity Reviews, 12(5): e173–82.
32. Maller C, Townsend M, Brown P & St Leger L (2002). Healthy parks healthy people: the health benefits of contact with nature in a part context. A review of current literature. Melbourne: Deakin University.
33. NSW Department of Health (2002). Walk it: active local parks. The effect of park modification on physical activity participation. Summary report. Sydney: NSW Health Department.
34. Bohn-Goldbaum EE, Phongsavan P, Merom D & Bauman AE (under review). Does playground improvement result in increased physical activity among children?257
35. Cohen DA, Golinelli D, Williamson S, Sehgal A, Marsh T & McKenzie TL (2009). Effects of park improvements on park use and physical activity: policy and programming implications. American Journal of Preventive Medicine, 37(6): 475–80.
36. Tester J & Baker R (2009). Making the playfields even: evaluating the impact of an environmental intervention on park use and physical activity. Preventive Medicine, 48: 316–20.
37. Cohen DA, Marsh T, Williamson S, Pitkin Derose K, Martinez H, Setodji C & McKenzie TL (2010). Parks and physical activity: why are some parks used more than others? Preventive Medicine, 50: S9–S12.
38. Turrell G, Kavanagh AM, Draper G & Subramanian SV (2007). Do places affect the probability of death in Australia? A multilevel study of area-level disadvantage, individual-level socioeconomic position and all-cause mortality, 1998–2000. Journal of Epidemiology and Community Health, 61(1): 13–19.
39. Kavanagh AM, Goller JL, King T, Jolley D, Crawford D & Turrell G (2005). Urban area disadvantage and physical activity: a multilevel study in Melbourne, Australia. Journal of Epidemiology and Community Health, 59(11): 934–40.
40. Coen SE & Ross NA (2006). Exploring the material basis for health: characteristics of parks in Montreal neighborhoods with contrasting health outcomes. Health & Place, 12(4): 361–71.
41. Giles-Corti B & Donovan RJ (2002). Socioeconomic status differences in recreational physical activity levels and real and perceived access to a supportive physical environment. Preventive Medicine, 35(6): 601–11.
42. Moore LV, Diez Roux AV, Evenson KR, McGinn AP & Brines SJ (2008). Availability of recreational resources in minority and low socioeconomic status areas. American Journal of Preventive Medicine, 34(1): 16–22.
43. Timperio A, Ball K, Salmon J & Crawford RD (2007). Is availability of public open space equitable across areas? Health & Place, 13: 335–40.
44. McLaren L, McIntyre L & Kirkpatrick S (2010). Rose’s population strategy of prevention need not increase social inequalities in health. International Journal of Epidemiology, 39(2): 372–77.
45. Centers for Disease Control and Prevention (CDC) (2010). Guide to community preventive services: promoting physical activity: Environmental and policy approaches [Online]. Available: www.thecommunityguide.org/pa/environmental-policy/index.html [Accessed 23 July 2011].
46. Rangan A, Kwan J, Flood V, Louie J & Gill T (2011). Changes in ‘extra’ food intake among Australian children between 1995 and 2007. Obesity Research & Clinical Practice, 5: e55–e63
47. Rangan AM, Randall D, Hector DJ, Gill TP & Webb KL (2009). Consumption of ‘extra’ foods by Australian children: types, quantities and contribution to energy and nutrient intakes. European Journal of Clinical Nutrition, 62(3): 356–64.
48. Story M, Kaphingst KM, Robinson-O’Brien R & Glanz K (2008). Creating healthy food and eating environments: policy and environmental approaches. Annual Review of Public Health, 29: 253–72.
49. Morland K, Wing S & Diez Roux A (2002). The contextual effect of the local food environment on residents’ diets: the atherosclerosis risk in communities study. American Journal of Public Health, 92(11): 1761–67.258
50. Burns CM, Gibbon P, Boak R., Baudinette S & Dunbar JA (2004). Food cost and availability in a rural setting in Australia. Rural Remote Health, 4(4): 311.
51. Cummins S & Macintyre S (2002). A systematic study of an urban foodscape: the price and availability of food in greater Glasgow. Urban Studies, 39(11): 2115–30.
52. Macintyre S (2007). Deprivation amplification revisited; or, is it always true that poorer places have poorer access to resources for healthy diets and physical activity? International Journal of Behavioral Nutrition and Physical Activity, 4(32).
53. Cummins S, Smith DM, Taylor M, Dawson J, Marshall D, Sparks L & Anderson AS (2009). Variations in fresh fruit and vegetable quality by store type, urban-rural setting and neighbourhood deprivation in Scotland. Public Health Nutrition, 12(11): 2044–50.
54. Giskes K, Turrell G, van Lenthe FJ, Brug J & Mackenbach J P (2006). A multilevel study of socioeconomic inequalities in food choice behaviour and dietary intake among the Dutch population: the GLOBE study. Public Health Nutrition, 9(1): 75–83.
55. Wrigely N, Warm D & Margetts B (2003). Deprivation, diet and food retail access: findings from the Leeds ‘Food Deserts’ study. Environment and Planning, 35: 151–88.
56. Cummins S, Petticrew M, Higgins C, Sparks L & Findlay A (2004). Reducing inequalities in health and diet: the impact of a food retail development. A pilot study. London: MRC Social and Public Health Sciences Unit.
57. Boone-Heinonen J, Gordon-Larsen P, Kiefe CI, Shikany JM, Lewis CE & Popkin BM (2011). Fast food restaurants and food stores longitudinal associations with diet in young to middle-aged adults: the CARDIA Study. Archives of Internal Medicine, 171(13): 1162–70.
58. Burns C & Inglis A (2007). Measuring food access in Melbourne: access to healthy and fast food by car, bus and foot in Melbourne. Health & Place, 13: 877–85.
59. Blewett N, Goddard N, Pettigrew S, Reynolds C & Yeatman H (2011). Labelling logic: review of food labelling law and policy [Online]. Available: www.foodlabellingreview.gov.au/internet/
foodlabelling/publishing.nsf/content/labelling-logic. [Accessed 4 May 2011].
60. Gorton D (2007). Nutrition labelling: update of scientific evidence on consumer use and understanding of nutrition labels and claims [Online]. Available: www.foodsafety.govt.nz/elibrary/industry/signposting-nutrition-study-research-projects/signs-literature-review-report_final-2.pdf [Accessed 5 May 2011].
61. Malam S, Cleg S, Kirwan S & McGinigal S (2009). Comprehension and use of UK nutrition signpost labelling schemes. London UK: Food Standards Agency.
62. Vyth EL, Steenhuis IH, Roodenburg AJ, Brug J & Seidell JC (2010). Front-of-pack nutrition label stimulates healthier product development: a quantitative analysis. International Journal of Behavioral Nutrition and Physical Activity, 7: 65.
63. National Heart Foundation of Australia (2010). Rapid review of the evidence: the need for nutritional labelling on menus. National Heart Foundation of Australia.259
64. Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V & Chisholm D (2010). Tackling unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. The Lancet, 376(9754): 1775–84.
65. Vos T, Carter R, Barendregt J, Mihalopoulos C, Veerman JL, Magnus A, Cobiac L, Bertram MY, Wallace AL & ACE-Prevention Team (2010). Assessing cost-effectiveness in prevention (ACE-Prevention): final report. Melbourne: Deakin University and Brisbane: University of Queensland.
66. World Health Organization (2010). Set of recommendations on the marketing of foods and non-alcoholic beverages to children. Geneva: World Health Organization.
67. National Preventive Health Taskforce (2009). Australia: the healthiest country by 2020. The report of the National Preventative Health Strategy: the roadmap for action. Canberra: Commonwealth of Australia.
68. National Preventative Health Taskforce (2010). Taking preventative action. A response to Australia: the healthiest country by 2020. The report of the National Preventative Health Strategy: the roadmap for action. Canberra: Commonwealth of Australia.
69. Hebden LA, King L, Grunseit A, Kelly B & Chapman K (2011). Advertising of fast food to children on Australian television: the impact of industry self-regulation. Medical Journal of Australia, 195(1): 20–24.
70. King L, Hebden L, Grunseit A, Kelly B, Chapman K & Venugopal K (2011). Industry self-regulation of television food advertising: Responsible or responsive? International Journal of Pediatric Obesity, 6(2–2): e390–e98.
71. Hebden L, King L, Kelly B, Chapman K & Innes-Hughes C (2010). Industry self-regulation of food marketing to children: reading the fine print. Health Promotion Journal of Australia, 21(3): 229–35.
72. Hebden L, King L, Kelly B, Chapman K & Innes-Hughes C (2010). Regulating the types of foods and beverages marketed to children: how useful are food industry commitments. Nutrition & Dietetics, 67(4): 258–66.
73. Maibach EW, Abroms LC & Marosits M (2007). Communication and marketing as tools to cultivate the public’s health: a proposed ‘people and places’ framework. BMC Public Health, 7: 88.
74. Rose G (1992). The strategy of preventive medicine. Oxford: Oxford University Press.
75. Australian Government. Swap it, don’t stop it [Online]. Available: www.swapit.gov.au [Accessed 23 July 2011].
76. Wallack W, Dorfman L, Jernigan D & Themba M (1993). Media advocacy and public health: power for prevention. Newbury Park: Sage.
1 Prevention Research Collaboration, Sydney School of Public Health, University of Sydney.