6
Vaping to quit: the latest mass distraction
Electronic cigarettes (e-cigarettes or ECs) and heat-not-burn nicotine vaping products (NVPs, which include ECs) have become immensely popular in some parts of the world since their first appearance in China in 2004. In the UK and USA, they are now the most common aid being used in cessation attempts (West, Kale et al. 2021). Market analysts Grand View Research estimated the global vape market size at US$15.04 billion in 2020 and expected this to expand at a compound annual growth rate of 28.1% from 2021 to 2028 (Grand View Research 2021). The boundless hype megaphoned by NVP marketers and enthusiasts about these products is that they are as near as possible to being perfectly benign health-wise; that they are peerless in their effectiveness as a means of quitting smoking; that they are a massively disruptive product in the way that digital cameras were to film cameras and electric vehicles are fast becoming to fossil-fuel-powered cars; and that they are capable of saving a billion lives this century, in people who are forecast to die from smoking (A billion is the number of smokers who’ve been estimated will die from smoking-caused diseases by the end of this century) (Peto and Lopez 2001).
That final modest claim assumes that all the world’s smokers would permanently switch to NVPs and never return to smoking, with combustible tobacco use disappearing without a trace, and that these products will also prove to be as benign as fairy dust into the long-term. As I will discuss in this chapter, widespread sightings of porcine aviation seem about as likely.
Big Tobacco butts in
All transnational tobacco companies have lost no time investing heavily in the development and marketing of NVPs (Tobacco Tactics 2020a). Some of these companies have made statements that they hope to one day stop selling combustible tobacco products. But tellingly, unlike the car manufacturing industry where ten companies have now announced dates for them to stop manufacturing fossil-fuelled cars (Nicholson 2021), no tobacco company has set a target date for the end of cigarettes. And just as tellingly, they continue to do all they can to maximise cigarette sales and as they’ve done for 70 years, thwart any evidence-based government policies which seriously threaten to put a brake on the uptake of smoking or accelerated quitting.
Far from turning off its efforts to produce and market cigarettes, Philip Morris International (PMI) continues to expand its cigarette business wherever it can. In March 2018, PMI opened a new factory in Tanzania with capacity to produce 400 million cigarettes a year “to cater for the local and international market” (Tanzania Invest 2018). In October 2021, Turkish conglomerate Sabanci Holding took steps to turn over its shares in Philip Morris Sabanci Cigarette and Tobacco Inc (PHILSA) and Philip Morris Sabanci Marketing and Sales Corp (PMSA) to its parent company, PMI, thus consolidating PMI’s interests in tobacco (Daily Sabah 2021).
In Indonesia, the world’s fourth most populous nation with huge rates of male smoking and feeble tobacco control, PMI owns the Sampoerna cigarette company but local sales of its IQOS NVP are very small. PMI’s president for South and Southeast Asia, Stacey Kennedy, explained on PMI’s website:
If we packed up and left Indonesia tomorrow it doesn’t change anything for smokers. They just pick up a different cigarette. Cigarettes don’t go away until we give adult smokers an alternative … How we go from a small scale to a large scale is the journey that we’re trying to tackle now. We’re absolutely on the path to transition from conventional cigarettes to smoke-free products in Indonesia, just like we are everywhere else in the world. It takes time. Every country’s path is unique, because there’s different levels of awareness and support, country by country (Kennedy 2019).
Kennedy was adamant that it’s “simply not true” that PMI only focuses on its heated tobacco products in wealthy nations:
We want to bring smoke-free alternatives to all adult smokers in Indonesia over time. That’s a pretty big ambition and it starts with being able to understand what adult smokers need and want … I can absolutely tell you that I spend the vast majority of my time focused on Indonesia and other countries in Southeast Asia and how we can convince adult smokers who won’t otherwise quit to switch to our reduced-risk products.
But Kennedy’s words are hard to reconcile with what PMI does in concert with other cigarette manufacturers in Indonesia when it comes to local tobacco control policies. In Indonesia, Gaprindo, the white (non-kretek) cigarette manufacturers association, represents the interests of transnationals like PMI, British American Tobacco (BAT) and Japan Tobacco International (JTI). Gaprindo routinely lobbies to oppose tobacco control policies like tax increases, as does the tobacco industry globally. In November 2018, it fought advertising bans and opposed tax increases (Cahya 2018). The head of Gaprindo said that the cigarette industry has in the past few years experienced a sales volume decline of 1–2%. In 2015, Gaprindo said, “Increasing excise tax on cigarettes twice a year will just harm the [tobacco] industry growth” (Amin 2015).
PMI has even gone as far as saying that they want their customers to stop using all forms of nicotine: “To be clear, PMI’s core message is: For adults who use nicotine in any form it is best to quit completely” (Kary and Gretler 2020). Here, we are meant to believe that the company wants its cigarette customers to stop smoking and switch to its heat-not-burn IQOS brand (which contains tobacco). But it says it wants even these customers (“it is best”) to also quit IQOS. This sounds as credible as a motor vehicle company urging owners of its petrol-powered vehicles not just to switch to its fully electric models, but to also then abandon those and not own cars at all. Only a tobacco company could have the weapons-grade gall to make such a statement publicly.
In a 2019 presentation to investors, BAT emphasised that dual and poly-using next generation product (NGP) users were of vital importance to its mission. Sixty-five percent of EC users and 55% of heated tobacco product (HTP) users are dual users. These products allowed nicotine “moments being regained” in places where “smoking is not allowed or socially unacceptable, such as in a shared office, at home with family, or in public social spaces” (Tobacco Tactics 2021). In 2018, BAT’s boss, Nicandro Durante, said that dual use had become “the key consumer dynamic”, growing from 13% to 23% in less than one year. Another BAT presentation identified most popular “new occasions” for EC users were “when I can’t smoke cigarettes” (86%), “in the car” (62%) and “inside pubs and restaurants” (47%) (Durante 2018).
So BAT, like all tobacco companies, knows very well that its bread is being buttered far more by the pursuit of dual and poly NVP and NGP use than by just concentrating on cigarettes. And like all of them, it’s very happy to do whatever it can to maximise sales of all its addictive products.
In late 2021, the US Federal Trade Commission published its annual report on total cigarette sales (including promotional giveaways) and marketing expenditure in the USA, drawing on data supplied by the four largest tobacco companies operating there (United States Federal Trade Commission 2021). US tobacco sales were up for the first time in 20 years with 203.7 billion cigarettes sold or given away. The US tobacco industry has been experiencing an unstoppable haemorrhaging of sales for over 20 years. The small 2020 rise needs to be seen in context of the 48.9% continual fall that had been happening since 2001.
The industry does all it can to stem this bleeding. Its advertising and promotional expenditures rose 2.8% in 2020 to reach US$7.84 billion, with the biggest spend being discounts paid to cigarette wholesalers and retailers (a whopping 88.5% of all promotional expenditure) to keep the price of cigarettes as low as possible for smokers to encourage sales. Remember this next time you hear anyone in the tobacco industry unctuously intoning that they want to get out of selling combustible tobacco while vaping proliferates.
Those who promote vaping typically focus their pitch around five arguments for why they believe NVPs are a revolutionary disruptive technology which promises to reduce the galactic harm caused by smoking:
- NVPs are all but 100% safe (“E-cigarettes are about as safe as you can get … E-cigarettes are probably about as safe as drinking coffee. All they contain is water vapour, nicotine and propylene glycol [which is used to help vaporise the liquid nicotine]” (Hickman 2013).
- It’s not too early to declare that NVPs will not have long-term serious health consequences.
- Nearly all teenagers who vaped before they started smoking would have smoked anyway.
- Flavours are a vital factor explaining the popularity of vaping and therefore governments should let a million flavours bloom with minimal regulation.
- NVPs are peerless as an effective way of helping smokers quit permanently.
Pulling all these together, who could possibly be in any doubt that in NVPs we have the ingredients for a major milestone in the entire history of public health. Or so the hype goes. Indeed, one vaping champion, the hyperbolic David Nutt, has gone as far as declaring breathlessly that e-cigarettes are “the most significant advance [in medicine] since antibiotics” (National Institute for Health Innovation 2013); are “the greatest health advance since vaccinations” (BBC News 2014); and that those rejecting the opportunity of harm reduction from vaping are engaging in “perhaps the worst example of scientific denial since the Catholic Church banned the works of Copernicus in 1616” (Caruana 2020). While I’ve yet to see a single authoritative source endorse or even repeat any of these comparisons, Nutt was apparently being serious.
The focus of this book is smoking cessation, the fifth of the pitches for vaping I listed above. So the bulk of this chapter will examine the evidence for this claim, highlighting the conclusions of reviews of recent evidence for smoking cessation which have been published since 2017; the evidence for cessation from randomised controlled trials; and papers coming out of the large US Population Assessment of Tobacco and Health (PATH) prospective cohort study which commenced in 2013 and provides the most important data on transitions in nicotine use across the years since (Hyland, Ambrose et al. 2017).
I’ll look at challenges in assessing the role played by vaping in reducing smoking at the population level, when many other variables known to put downward pressure on smoking are also in play at the same time. I’ll also consider the question of whether vaping might actually hold more people in smoking, than providing a large-scale off-ramp out of it. If this were the case, the interests of the tobacco industry in eagerly promoting NVPs would be obvious. I’ll also look at evidence that vaping reduces smoking frequency (how many cigarettes are smoked each day) in those who keep smoking while vaping (dual users) and whether reduced use actually reduces harm in those who cut down rather than quit all smoking.
But before turning to these questions, let’s briefly look at the four other core claims about NVPs.
“95% less dangerous than smoking”
A claim relentlessly asserted by vaping advocates is that NVPs are far less dangerous than smoking, most commonly phrased as “95% less dangerous” than smoking. This figure emerged from a meeting held in London in 2014 of twelve selected participants, several of whom had track records as tobacco harm-reduction advocates. Some had tobacco industry connections (Gornall 2015). David Nutt chaired the group. The published paper in which this resoundingly large, unforgettable number first appeared provided no data or calculations on how it was arrived at, beyond describing a process where the participants ranked different nicotine products against cigarettes, using 16 criteria on harm (Nutt, Phillips et al. 2014).
Specifically excluded from the list of harms were drug-specific and drug-related mental impairment so that the potential of various nicotine delivery devices to initiate and perpetuate nicotine addiction was not included in the assessment, despite tobacco use disorder or dependence being included in the International Classification of Diseases (ICD) of the World Health Organization, and the Diagnostic and statistical manual of mental disorders (DSM), compiled by the American Psychiatric Association.
However, deep in the paper’s discussion section, the authors stated, perhaps at the insistence of reviewers’ and editors’ comments, “A limitation of this study is the lack of hard evidence for the harms of most products on most of the criteria” used to rank the harmfulness of different nicotine delivery products.
Let’s pause here and roll that sentence around in our minds again. In my over 40 years of academic life in public health, including editing a research journal (Tobacco Control) for 17 of these which currently has the highest impact factor in its field, and having reviewed hundreds of research papers, I don’t recall ever reading such a deeply self-eviscerating “Actually, we have almost no hard evidence” caveat about the very foundations of an exercise in supposed scientific risk assessment. This caveat is frankly a public suicide note for the credibility of the paper’s central take-home message. But it is not an admission which has given NVP “true believers” even the slightest pause to keep megaphoning it as much as possible over the past seven years.
With others, I have critiqued the provenance of the “95% less dangerous” statement in the American Journal of Public Health (Eissenberg, Bhatnagar et al. 2020) and in greater detail in my blog (Chapman 2019). I showed how it has been uncritically repeated and even pushed beyond 95% by some, with all referencing leading back to the original Nutt group report with its sweeping “there’s no hard evidence” caveat. A factoid is an item of unreliable information that is reported and repeated so often that it becomes accepted as fact. The 95% claim is a vampire-like factoid which just won’t die and derives its status from its mass repetition as an article of faith in what I’ve often heard described as vaping theology.
Too soon to know the true health risks of vaping
When confronted with their 95% emperor’s lack of evidential clothing, vaping advocates frequently retort, “Well, if it’s not 95% safer, what’s your figure then?” Those who believe this question can actually be answered today could only be ignorant of the nature of risk assessment of chronic diseases and the history of our evolving understanding of the risks of smoking. Or perhaps they believe that scientific risk assessment is properly approached by guesswork.
Cigarette use exploded at the beginning of the 20th century after mechanisation in factories replaced handmade cigarettes. This made smoking very affordable to even those on the lowest incomes. But tobacco-caused diseases didn’t start showing up in large numbers until 30–40 years later. US surgeon Alton Ochsner, recalling attendance at his first lung cancer autopsy in 1919, was told he and his fellow interns “might never see another such case as long as we lived”. He saw no further cases until 17 years later in 1936 – and then saw another nine cases in six months (Ochsner 1971). Since the 1960s, lung cancer has been by far the world’s leading cause of cancer death with 18% of all cancer deaths in 2020, ahead of the next most frequent killer, liver cancer, with 8.3% (Sung, Ferlay et al. 2021).
The chronic diseases caused by smoking take many years before manifesting clinically. They are not like infectious, communicable diseases such as COVID-19, influenza or HIV where there is typically a very short period between exposure to the infectious agent and the onset of symptoms and sometimes death. Instead there are long latency periods that can stretch for several decades when smokers may not have any signs or symptoms of emerging disease (Smith, Imawana et al. 2021).
The incidence of lung cancer rose rapidly in the decades 1930–80 but it was not until 1950 that seriously compelling case-control evidence was published in the USA (Wynder and Graham 1950) and England (Doll and Hill 1950). These reports were foundational in the emerging consensus that long-term smoking caused lung cancer. Knowledge about smoking’s causal role in many other diseases followed and continues to consolidate, with the smoking attributable death rate increasing in recent years from half of long-term smokers (Doll, Peto et al. 2005) to two in three (Banks, Joshy et al. 2015).
If any scientist had declared in 1920 that cigarette smoking was all but harmless, as vaping advocates insist today about NVPs, history would have judged their call as heroically and dangerously incorrect. But this is the cavalier call that many vaping advocates routinely make, after just 10 years or so of widespread use in some nations. For example, English vaping advocate Clive Bates put it simply in a 2017 interview produced for the government agency Public Health England (PHE): “Almost none of the [news media] stories holds any water or should give anyone any cause for concern” (Public Health England 2017). And Professor Robert Beaglehole went a step further in a video interview with a vaping advocacy group, at one point referring to “the supposed harm of nicotine and vaping” while theatrically gesturing air quotes around “supposed harm”. He then said, “A lot of that information is incorrect. All of it is incorrect. And based on very poor science and vested interests” [my emphasis] (Chapman 2021).
All of it is incorrect? All of it? So any published evidence that has concluded that there are any concerns about vaping being harmful or not very effective in helping smokers quit it is all wrong, apparently.
With vaping having been around in large numbers for only about ten years, it is predictable and unsurprising that we have as yet seen little clinical disease caused by e-cigarette vaping. As acknowledged in 2021 by 15 presidents of the global Society for Research on Nicotine and Tobacco, “High-quality clinical and epidemiological data on vaping’s health effects are relatively sparse. There are no data on long-term health effects, reflecting the relative novelty of vaping and the rapid evolution of vaping products. Determining even short-term health effects in adults is difficult because most adult vapers are former or current smokers” (Balfour, Benowitz et al. 2021). However, recent reviews of cardio-respiratory impacts of vaping may be pointing to sick canaries in this coalmine (e.g. Tsai, Byun et al. 2020, Wehrli, Caporale et al. 2020, Keith and Bhatnagar 2021).
Professor John Britton from the University of Nottingham acknowledged this in the same 2017 PHE compilation interview as Clive Bates’ statement, saying, “ Inhaling vapour many times a day for decades is unlikely to come without some sort of adverse effect. And time will tell what that will be” (Public Health England 2017).
A colleague of mine, Sydney respiratory physician Professor Matthew Peters, summarised recent research this way:
Ween et al. recently reported findings of a carefully conducted study on the effects of e-liquid exposure in human bronchial epithelial cells (Ween, Hamon et al. 2020). There were three key findings. E-cigarette (EC) liquids, with a variety of constituents, induce damage that manifests as necrosis and apoptosis; macrophage efferocytosis, an adaptive mechanism that clears apoptotic cells, is compromised; and purchasers of EC liquids can have no confidence in the constituents that they are exposing their lungs to – with three versions of apple flavour having very different chemical mixes. The observations of Ween et al. have even greater pertinence after the report of histopathology from 17 cases within the current outbreak (Butt, Smith et al. 2019). Open biopsy findings suggest that the dominant pathology is a form of airway-based chemical pneumonitis and not exogenous lipoid pneumonia as previously believed by some (Peters 2020).
These findings complement an NIH-funded comprehensive 2017 review by Chun et al. on the effects of EC on the lung, which examined a combination of in vivo and in vitro studies (Chun, Moazed et al. 2017). Since that publication, we have also seen the seminal work of Ghosh et al. who observed airway inflammation in a man in vivo, describing the proteomic characteristic of bronchial tissue in smokers, EC users and controls (Ghosh, Coakley et al. 2018). In summary, considering significant positive and negative changes, there were 292 changes seen with smoking, of which 78 were also seen with EC use. Importantly, there were 113 separate proteomic changes that occurred only with EC use. This would not be unexpected by an open mind because the nature of the lung exposure is very different.
A 2020 New England Journal of Medicine report of serious pulmonary disease in two US states in 53 vapers, with a median age of just 19, found that 17% of these patients reported vaping only nicotine products (Layden, Ghinai et al. 2020). British NVP advocates were quick to point out that none of these cases were being reported in the UK where vaping is also prevalent. Soon afterwards the British Medical Journal (BMJ) published a case report of a young woman with respiratory failure from lipoid pneumonia, suspected of being caused by her vaping (Viswam, Trotter et al. 2018). In October 2021, the Medical Journal of Australia published a case report of a 15-year-old girl hospitalised with diagnostic criteria consistent with Electronic Cigarette or Vaping Product Use-Associated Lung Injury (EVALI) (Chan, Kiss et al. 2021). She had vaped two to three times a week for seven months, had smoked cannabis through a water pipe and also smoked cigarettes, like a majority of vapers do. But she had never vaped cannabis and her vaping device contained no traces of cannabis nor vitamin E acetate, agents known to be present in many, but not all, cases of EVALI (Winnicka and Shenoy 2020).
In February 2022, ABC TV in Australia reported on an autopsy conducted on a 71-year-old man who had switched to daily vaping 10 years earlier and had died after collapsing and being put into a coma with acute lung failure. The autopsy described “acute lung injury superimposed on chronic lung disease and a probable cause of EVALI – meeting three of the four criteria”. The man’s intensive care doctor described “huge cystic lesions at the apex of the lung” and noted that with emphysema, the typical presentation of lung injury was throughout the lung (Atkin 2022).
When many have pointed out this fundamental “too soon to know” problem, vaping defenders snort derisively that toxicological science has progressed exponentially in the years since the connection of smoking with cancer was first authoritatively established. The implication here is that we can now tell very early with a high degree of certainty if a drug or chemical combinations such as those found in NVPs are likely to cause disease down the track.
That certainty would be informed by all that advanced crystal-balling toxicology capable of early detection of long-term risk so brilliantly that between 1953 and 2014, 462 drugs initially assessed as being likely to be safe and let into the market have been withdrawn with some causing very serious health problems or death (Onakpoya, Heneghan et al. 2016). Remember the global thalidomide birth defects tragedy? (Sjostrom and Nilsson 1972).
All but the most impoverished and chaotic nations have drug assessment, scheduling, adverse event reporting, and the possibility of recall and bans because pre-registration drug trials can never provide data on the consequences of long-term use. That of course is not a sensible reason to ban all new drugs, but it is the primary reason why new drugs are almost invariably scheduled as prescription-only so that monitoring of any adverse reactions can be better undertaken. Many prominent vaping advocates have been stridently opposed to NVPs being scheduled as prescription items. They appear to embrace a peculiar kind of regulatory exceptionalism, strongly supporting drug regulation in general but not when it comes to vaping.
In 2017 vaping activists on social media were jubilant about a 3.5 year follow-up study of just nine subjects (with another seven having dropped out) which – hey presto – showed no “long term” ill-effects (Polosa, Cibella et al. 2017). “Case closed: study shows no lung damage from vaping” gloated one report on a pro-vaping channel (Stafford 2017). Such a baby-steps follow-up between exposure and pathology compares with the 9 to 11-fold greater 30–40 years that passed before the huge upswing in smoking in the first decade of the 20th century began to show lung cancer in case-control studies in the early 1950s.
A good example of the common “nothing to worry about” promotion of vaping can be seen in the online promotion in Figure 6.1 promising “risk free” vaping, with one mouse click past the first page we find a remarkably self-contradictory sentence that vapers can “entirely avoid the harm” while “lessen[ing] the possibility of inducing danger on your lungs”. Reckless calls to just allow unregulated NVPs to flood corner stores and be promoted with advertising like that is the sort of risk assessment we are supposed to embrace by flatulent arguments that the risks of vaping are already known.
If NVPs are really so safe and so effective, their manufacturers would surely have nothing to fear by applying for registration through regulatory bodies like the Australian Therapeutic Goods Administration (TGA). Why is it then, that no such applications have been received? What might these manufacturers know or fear that the TGA’s assessment process might conclude?

Figure 6.1 Online ad for “risk free vaping”.
PATH data on toxicant exposure: never-tobacco users vs. smokers vs. exclusive vapers vs. dual users
Information of immense importance to the debate about the net contribution of vaping to toxicant exposure was published in 2018 using data obtained from the US longitudinal PATH study (Goniewicz, Smith et al. 2018). The authors compared concentrations of tobacco-related toxicant biomarkers among e-cigarette users with those observed in cigarette smokers, dual users of e-cigarettes and cigarettes, and those who had never used tobacco in any form. They compared mean concentrations of 50 individual biomarkers from five major classes of tobacco product constituents: nicotine, tobacco-specific nitrosamines (TSNAs), metals, polycyclic aromatic hydrocarbons (PAHs) and volatile organic compounds (VOCs). Following is a summary of their main findings.
Never-tobacco users vs. exclusive EC users
Those who had never used tobacco in any form had significantly lower concentrations of all major nicotine metabolites and total nicotine equivalents, all TSNAs, four metals, one PAH and four VOCs than did exclusive vapers. These included:
- NNAL (the tobacco-specific carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol): 81% less
- Metal exposure: lead (19% less), cadmium (23% less)
- Pyrene: 20% less
- Acrylonitrile: 67% less
Exclusive EC users vs. exclusive smokers
Exclusive EC users had significantly lower concentrations of all major nicotine metabolites, two minor tobacco alkaloids, all TSNAs, one metal (cadmium), all PAHs and 17 VOCs (markers for toluene, benzene and carbon disulfide) than did exclusive smokers. These included:
- Total nicotine equivalents: 93% less
- NNAL: 98% less
- Cadmium: 30% less
- Naphthalene: 62% less
- Pyrene: 47% less
- Acrolein: 60% less
- Acrylonitrile: 97% less
Dual users vs. exclusive cigarette smokers
Claims are often made that dual users replace some of the cigarettes they once smoked with ECs and are thereby predicted to be reducing their total toxicant load. But contrary to that claim, dual users in this study were found to have significantly higher concentrations of most biomarkers, including most major nicotine metabolites, 3 TSNAs, two metals, five PAHs and 13 VOCs than exclusive smokers. These included:
- Total nicotine equivalents: 36% more
- NNAL: 23% more
- Pyrene: 15% more
- Acrolein: 10% more
- Acrylonitrile: 15% more
- Lead and cadmium levels were equivalent
So in summary, if you have never used tobacco in any form, unsurprisingly you are likely to have far lower biomarkers for tobacco use than those who use ECs. If you exclusively use ECs, you’ll have far lower tobacco toxicant levels than if you smoke. And if you both smoke and vape (dual use), you’ll have higher levels than those who only smoke. So if dual use is the Mount Everest of toxicant exposure, then smoking is the K2 exposure, vaping is the Matterhorn and never smoking or vaping is the toxicant exposure at sea level.
Adding to this, another paper using PATH data (Christensen, Chang et al. 2021) found that dual users have a greater concentration of an oxidative stress marker, F2-isoprostane, than smokers. Exclusive EC users have biomarker concentrations at similar levels to those of former smokers, and lower than those of exclusive cigarette smokers.
Johns Hopkins University researchers applied liquid chromatography–high-resolution mass spectrometry (LC–HRMS) and chemical fingerprinting techniques to characterise e-liquids and aerosols from a selection of popular EC products (Mi-Salt™, Vuse™, Juul™ and Blu™) (Tehrani, Newmeyer et al. 2021). They found nearly 2,000 chemicals in these products, the vast majority of which were unidentified. Six potentially hazardous additives and contaminants, including the industrial chemical tributylphosphine oxide were identified. The authors noted, “Existing research that compared e-cigarettes with normal cigarettes found that cigarette contaminants are much lower in e-cigarettes. The problem is that e-cigarette aerosols contain other completely uncharacterized chemicals that might have health risks that we don’t yet know about” (Johns Hopkins University 2021).
Many vaping advocates appear to believe they are on a messianic mission to save a billion lives. All tobacco companies now marketing NVPs are delighted to buy into that framing of what vaping is all about, while just down the corridor in their tobacco divisions they continue trying to maximise demand for the cigarettes that will cause the same billion deaths they claim vaping could prevent.
Armed with that moral imperative, like all evangelists they believe that no impediment should be placed in the way of their lifesaving work. But medicine of course has a very long history of claims being made by purveyors of a multitude of miracle cures who also believe their crusades are far too important to be regulated by the dead hand of bureaucracy in government agencies (Barker Bausell 2007). Most people readily understand why consumer protection laws often include specific provisions about outlawing health and medical claims for which there is little or no evidence. Quack claims for treatments for cancer, HIV/AIDS, COVID-19, asthma and many other life-threatening diseases have long been exposed and prosecuted by governments or their drug regulatory agencies.
But NVP advocates constantly make claims for both the safety and the efficacy of vaped products, despite them never having been declared as such by any regulatory agency. In October 2021, the US Food and Drug Administration (USFDA) announced that for the first time it had authorised the marketing of a limited number of NVPs. In doing so, however, the USFDA was explicit that about what this authorisation did not mean:
While today’s action permits the tobacco products to be sold in the US, it does not mean these products are safe or “FDA approved”. All tobacco products are harmful and addictive and those who do not use tobacco products should not start (US Food and Drug Administration 2021b).
In 2021 Australia’s TGA published a similar fundamental caveat on its new prescription-only access to NVPs (see Chapter 8):
There are currently no nicotine vaping products approved by the Therapeutic Goods Administration (TGA) and registered in the Australian Register of Therapeutic Goods (ARTG). Medicines that are not in the ARTG are known as “unapproved” medicines. There are established pathways for consumers to legally access unapproved nicotine vaping products, with a valid prescription, but these medicines have not been assessed by the TGA for safety, quality and efficacy (Therapeutic Goods Administration 2021b).
Safety and efficacy are the two core considerations on which drug regulation is based. But many vaping advocates believe their case should somehow place them above all this. There is much evidence of trying to walk on both sides of the street here. NVPs are better than NRT for cessation, they say, thus making a therapeutic claim. “Oh no, we are not making any therapeutic claim because NVPs are a ‘consumer product’, not a pharmaceutical product,” comes their reply. “Those using NVPs are not sick, so why should they be regulated by therapeutic agencies?” they continue. But those who take other smoking-cessation products like bupropion or varenicline aren’t “sick” either. Yet no one has called for these products to be sold over the counter at convenience stores.
However, the question of the safety of products claiming to help people stop smoking is tangential to the focus of this book: smoking cessation in real-world use. Readers wanting far more detailed information on developments are referred to authoritative reports like that of the 2018 doorstopper-sized report on ECs from the US National Academies of Sciences, Engineering and Medicine (National Academies of Sciences, Engineering and Medicine 2018). Among its conclusions on product safety were:
- There is substantial evidence that EC aerosols can induce acute endothelial cell dysfunction, although the long-term consequences and outcomes on these parameters with long-term exposure to EC aerosol are uncertain.
- There is substantial evidence that components of EC aerosols can promote formation of reactive oxygen species/oxidative stress. Although this supports the biological plausibility of tissue injury and disease from long-term exposure to EC aerosols, generation of reactive oxygen species and oxidative stress induction is generally lower from e-cigarettes than from combustible tobacco cigarette smoke.
- There is substantial evidence that some chemicals present in EC aerosols (e.g., formaldehyde, acrolein) are capable of causing DNA damage and mutagenesis. This supports the biological plausibility that long-term exposure to EC aerosols could increase risk of cancer and adverse reproductive outcomes.
Insignificant uptake by teens and no gateway to smoking?
A third platform of vaping theology sees vaping advocates dismiss all concerns about any reports of dramatic uptake of vaping by teenagers and those even younger by a three-step argument: first (as just discussed), vaping is all but benign, so there’s almost nothing to worry about when children vape. Second, nearly all children who take up smoking after first vaping would have taken up smoking anyway if NVPs had never appeared on the scene (so-called common liability theory) (Vanyukov, Tarter et al. 2012). And third, vaping “protects” children from starting to smoke, so we should perhaps even encourage it. This is an argument so bereft of evidence that it is usually only explicitly voiced by those from the twilight zone of vaping advocacy.
Australian vaping advocate Alex Wodak put much of this together in 2021 in a comment to the press when he likened teenage vaping to past harmless yoyo and hula-hoop fads: “In 2023 they’ll be on to hula hoops or yoyos, they’ll drop vaping. There are fads and fashions. Regular frequent vaping by young kids is not a problem and where young people vape, they have almost always been smokers first” (Hansen 2021). Wodak and other vaping advocates have often described concern about teenage vaping as a confected “moral panic”. They argue that it’s better that teenagers vape than smoke, that their vaping is preventing them from smoking, and so isn’t teenage vaping therefore nothing but positive?
This attempted framing is happening against a background where teenage smoking rates in nations like Australia have fallen to the lowest levels ever recorded, thanks to decades of success in tobacco control policies reducing uptake (Greenhalgh, Winstanley et al. 2019). As the tobacco industry watches a diminishing proportion of each birth cohort’s potential future smokers fail to take up smoking, the vital importance of addicting as many of these nicotine-naïve children to nicotine through vaping for the commercial viability of the tobacco industry is all too obvious and urgent (Chapman 2015).
New Zealand and Canada are cases in point. In New Zealand, following an unsuccessful 2018 challenge by the Ministry of Health over Philip Morris International’s plans to sell the NVP HEETS product (Reuters Staff 2018), the government was forced to allow the marketing of NVPs, including no age restrictions for purchase, no advertising constraints and no accountability for retailers.
Figure 6.2 shows what has been occurring with 14–15-year-olds’ regular smoking and vaping prevalence in New Zealand. Between 2012 and 2015, prior to the widespread availabilty of vaping, overall smoking fell by 21% from 6.8% to 5.5% and by 37% from 17.7% to 11.2% in Māori teenagers. But after the advent of vaping, the decline changed to a growth of 9% between 2015 and 2019, with Māori smoking rising 21%. While this was happening, regular vaping was rising dramatically: between 2015 and 2019, the prevalence of regular vaping rose 173% (5.4% to 12%) and by a roaring 261% in Māori teens (5.4% to 19.5%).
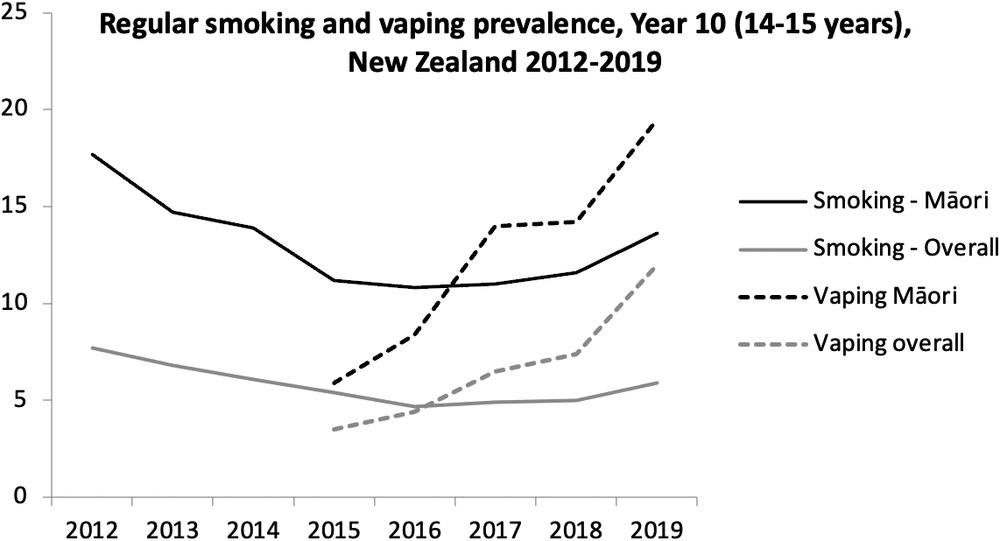
Figure 6.2 Regular smoking and vaping prevalence (per cent Y axis) Year 10 (14–15 years), New Zealand 2012–19 (Source: Action on Smoking and Health NZ 2021).
Canada similarly opened the EC floodgates in 2018. Statistics Canada released survey results from the national Canadian Tobacco and Nicotine Survey (CTNS) in July 2021. Although Canadian youth and young adults (aged 15 to 24) make up only 15% of the surveyed population, they accounted for 40% of those who vape. An estimated 425,000 teenagers vaped in Canada. About 1.46 million Canadians vaped in the previous month. Of these, one-third (485,100) were former smokers. The remainder were those who’d never smoked (438,500, 30%) or current smokers (532,400 dual users, 38%) (Statistics Canada 2021).
Immediately, both the New Zealand and Canadian governments started furiously backpedalling. From August 2021 new regulations in New Zealand “banned retailers such as dairies (small owner-operated convenience stores), service stations and supermarkets from selling vaping products in flavours other than tobacco, mint and menthol. Only specialist vape retailers will be able to sell other flavours. From 28 November, vaping and smoking in motor vehicles carrying children will be banned” (Verrall 2021). All advertising was prohibited, as was distribution of free NVPs and discounting (Ministry of Health New Zealand 2021b).
From the summer of 2019, only a year on from opening the floodgates and allowing a broad range of EC advertising, the Canadian government severely restricted promotions (Government of Canada 2021). In June 2021, Health Canada commenced public discussion of its intent to restrict vaping flavours options to tobacco and mint or menthol (Cision 2021) and reduced the maximum nicotine concentration in vaping liquids to 20 mg/ml in line with the European Union limit.
When asked about the rise in teenage vaping, extreme vaping advocates shrug with supreme indifference. More moderate advocates, intoning with socially responsible concern, typically call for policies that will target reducing youth uptake. Here, we encounter all manner of hopelessly naïve and discredited suggestions, such as retailer education, tougher and more explicit signage in shops advising that vaping is not for under 18s, marketing regulation that makes adult-directed advertising somehow magically invisible to youth, greater “education” and vigilance in ensuring that all online marketing is accompanied by site entry buttons requiring all potential visitors to declare that they are over 18 years old. That will stop them! All of these proposals had of course been trotted out for decades by the tobacco industry with its fingers firmly and cynically crossed behind their backs, knowing how ineffective each of these suggestions was (Knight and Chapman 2004).
As I’ll discuss in Chapter 8, requiring prescription authority to access NVPs combined with bans on all sales without prescription, all backed by seriously deterrent fines seem likely to be the only feasible ways of greatly reducing youth access.
While youth vaping rates are booming, there had been until recently (see Figure 6.2) no convincing evidence yet published of any substantial increase in uptake in adolescent smoking or stalling of its decline in any nation (although the very recent New Zealand data cited above are cause for concern). This has given succour to vaping advocates who like to point out that this lack of evidence is incompatible with the core prediction of gateway theory: if youth smoking rates are falling while vaping rates are rising, vaping cannot be acting in any significant way as a gateway. This argument is slippery with sophistry.
In a critique I wrote with Wasim Maziak and David Bareham of repudiations of the gateway hypothesis involving vaping and smoking, we pointed out:
declining trends of smoking among youth were apparent well before the introduction of e-cigarettes. Moreover, associations in population trends are known to be prone to the ecological fallacy; i.e. what is true at the population level may not be true at the individual level, especially when other population-level attributes are not considered (e.g. effective tobacco control policies). Specifically, the ecological argument relies on an assumption that the population net impact of any putative gateway effect of e-cigarette use would be larger than the combined net impact of all other policies, programs and factors which are responsible for reducing adolescent smoking prevalence (e.g. tobacco tax and retail price, measures of the denormalisation of smoking, exposure of children to adult-targeted quit campaigns, retail display bans, health warnings and plain packaging). This is an extremely high bar that gateway critics demand that anyone suggesting gateway effects needs to jump over. The combined impact of such factors in preventing uptake could, thereby, easily mask considerable smoking uptake that might not have occurred in the absence of e-cigarettes [my emphasis] (Chapman, Bareham et al. 2019).
Systematic reviews and meta-analyses on youth uptake
For this reason, cohort studies which follow the same individual adolescents across a number of years are of critical importance for they provide relevant data at the individual level as well as at the cohort group level. There have been several recent systematic reviews and meta-analyses on the question of whether young people who vape have a higher probability of later taking up smoking compared to those who never vape (Khouja, Suddell et al. 2020, O’Brien, Long et al. 2020, Yoong, Hall et al. 2021).
Khouja et al. included 17 studies in their meta-analysis and found strong evidence for an association between e-cigarette use among non-smokers and later smoking (OR: 4.59, 95% CI: 3.60 to 5.85) when the results were meta-analysed in a random-effects model.
The Irish Health Research Board, in an analysis of nine cohort studies conducted with follow-up periods between four and 24 months, also found that adolescents who ever used ECs were four times more likely to start smoking cigarettes. The strength of association was statistically significant across all primary research studies. They commented that “the findings build a case towards a causal relationship as the findings are consistent across all studies included in the meta-analysis” (O’Brien, Long et al. 2020).
Common liability theory holds that those who use drugs share common latent traits which account for or explain much of their drug use. This theory is probably the favourite objection used by vaping advocates who often crudely paraphrase it by saying that “kids who try stuff, will try stuff” or “kids who will smoke, will smoke”. This glib response has been repeatedly held aloft in arguments like an omnipotent crucifix before the evil gateway hypothesis vampire. It holds that children who are attracted to experiment with, say, vaping, may be more likely to have a propensity to be willing to try smoking and perhaps other “forbidden fruit” as well. These responses are voiced as self-evident truisms, with their circularity being seductive at first blush. However, any cessation researcher offering the equally trite “smokers who will quit, will quit” as a serious contribution to understanding the complexity of transitioning out of smoking, would be rightly pilloried for their primitive understanding of the complexities involved in reaching permanent smoking cessation.
There is a vast literature on the efficacy of smoking-cessation interventions where relevant mediating variables (for example: level of addiction, self-efficacy, levels of personal and professional support, planned versus unplanned and gradual versus rapid quit attempts) are measured, and then adjusted for in estimates of the contribution of the cessation drug or intervention. Yet common liability supporters argue that the hypothesis can explain all the main claims of the gateway hypothesis: all we need to say about anyone who smokes regularly is that they had a “propensity” to do so. If this hard determinism was all that was needed to be invoked in understanding smoking uptake, how then do we explain the dramatic falls in uptake that have been seen in nations which have robust tobacco control programs? What eroded that “propensity” to smoke so dramatically? Liability to nicotine dependence may well be a predisposing factor. But what of the known tractable reinforcing and enabling factors that tobacco control has so successfully identified and addressed over decades?
Most importantly and very awkwardly for this hypothesis, several longitudinal studies have reported that the strongest association between EC use and smoking initiation is among youth with the lowest risk of smoking (Primack, Soneji et al. 2015, Barrington-Trimis, Urman et al. 2016, Wills, Knight et al. 2017). Moreover, evidence using US National Youth Tobacco survey data shows that a third of youth who start with ECs have risk profiles that make them unlikely to start smoking (Dutra and Glantz 2017).
A 2021 paper in Addiction (Staff, Kelly et al. 2021) looked at adolescent EC use and tobacco smoking in the UK’s huge Millennium Cohort Study. It concluded:
Among youth who had not smoked tobacco by age 14 (n = 9,046), logistic regressions estimated that teenagers who used e-cigarettes by age 14 compared with non-e-cigarette users, had more than five times higher odds of initiating tobacco smoking by age 17 and nearly triple the odds of being a frequent tobacco smoker at age 17, net of risk factors and demographics.
Very importantly, the paper also knocked the stuffing out of the glib “kids who try stuff, will try stuff” common-liability theory adherents’ dismissal of the concern that vaping acts as training wheels for later smoking uptake. In their analysis, the authors controlled for a rich constellation of “propensity” to smoke factors that have been suggested by common liability theory adherents to predict smoking uptake in youth. These included parental educational attainment and employment status; parental reports of each child’s behaviour during the prior six months using the Strengths and Difficulties Questionnaire, with indicators of externalising behaviours (i.e. conduct problems, hyperactivity, inattention), and internalising behaviours (i.e. emotional symptoms, peer problems); parental smoking; whether a child spent time “most days” after school and at weekends hanging out with friends without adults or older youth present. Young people, via confidential self-reports, indicated whether they had ever drunk alcohol (more than a few sips), ever engaged in delinquency (e.g. theft, vandalism) and whether their friends smoked cigarettes. The authors concluded:
we found little support that measured confounders drove the relationships between e-cigarettes and tobacco use, as the age 14 e-cigarette and tobacco cigarette estimates barely changed with the inclusion of confounders or in matched samples. Furthermore, early e-cigarette users did not share the same risk factors as early tobacco smokers, as only half the risk factors distinguished e-cigarette users from non-users, whereas age 14 tobacco smokers were overrepresented on almost all the antecedent risk factors. If there was a common liability, we would expect similar over-representation for users of both forms of nicotine.
Flavours and vaping
NVPs have many aspects of appeal that differentiate them from cigarettes, NRT and other smoking-cessation pharmaceuticals. These include claims about them being much less harmful, being generally less expensive than cigarettes, being less astringently malodorous than cigarettes and providing continuity of the hand-to-mouth cigarette ritual. But perhaps the most prominent of the appeals is the cornucopia of beguiling flavours available to vapers which drives huge consumer demand, including among adolescents. I recently asked my 11-year-old granddaughter about what she thought attracted some of her Year 6 classmates to vaping. Instantly she replied, “You can get lemonade flavour!”
NVP flavours are very relevant to the focus of this book because if evidence demonstrated that vaping was an effective way to obtain a significant population level increase in quitting, and flavours were an important factor in attracting smokers to switch to vaping, then this would be an important argument in their favour.
However, we would still need to consider any potential downsides to the proliferation of vaping (such as non-smoking teenagers commencing vaping) in any risk–benefit analysis of their likely net effect. And here e-cigarette flavours wave a large red flag. A huge clue to one of these downsides lies in looking at the non-use of flavours in medicines that are inhaled daily all over the world.
Why aren’t asthma inhalers flavoured?
Australia, with a population of some 25 million, has about 2.7 million people living with asthma (Australian Institute of Health and Welfare 2020a), and some 464,000 with chronic obstructive pulmonary disease. Most of both groups use salbutamol inhalers (“puffers”) for relief, sometimes at lifesaving moments. But significantly, none of the asthma drugs that are inhaled come in flavours which might make them more palatable. Respiratory medicine colleagues tell me that many users, particularly children do not enjoy their distinctive medicinal taste. We’d therefore imagine that the manufacturers of inhaled medicines would jump at any opportunity to add flavours to puffers if this would encourage more people to use them when needed. It is unimaginable that pharmaceutical companies manufacturing them would not have long been aware of this unpleasant taste downside to their products and tried to find any way possible to have drug regulatory agencies allow them to add flavours as we see happen with infant cough mixtures, for example.
But none has done so.
One of the big reasons for this is undoubtedly because asthma products have to go through therapeutic goods regulation. The two considerations there are efficacy and safety. Efficacy refers to how well a drug performs in doing what it is supposed to do – so here, helping smokers quit. As we will see later in this chapter, when it comes to the question of how well vaping performs in helping smokers quit, the answer is ‘very poorly’. The pharmaceutical industry knows it would struggle to demonstrate that inhaling flavours is acceptably safe in the ways they would be used by vapers.
In 2014, there were already 7,764 unique vaping flavour names being sold online (Tierney, Karpinski et al. 2016). In 2016–17 this had more than doubled to 15,586 (Hsu, Sun et al. 2018). In 2017 Professor Robert West was confident this was unlikely to be a problem: “Now some concerns have been raised about the risk that might be attending to the flavourings in e-cigarette vapour but again, these are flavourings that have been tested and the concentrations are sufficiently low that we wouldn’t expect them to pose a significant health risk” (Public Health England 2017).
So is it indeed the case that these flavouring chemicals have all been “tested” and cleared by government food and drug regulatory bodies as safe to inhale? Well, no.
The peak flavour manufacturers association in the USA, the Flavor and Extracts Manufacturers Association (FEMA) stated in 2021:
- There is no apparent direct regulatory authority in the United States to use flavors in e-cigarettes. In this context, it is important to note that the “generally recognized as safe” (GRAS) provision in Section 201(s) of the Federal Food, Drug, and Cosmetic Act (FFDCA) applies only to food as defined in Section 201(f) of the Act.
- None of the primary safety assessment programs for flavors, including the GRAS program sponsored by the Flavor and Extract Manufacturers Association of the United States (FEMA), evaluate flavor ingredients for use in products other than human food. FEMA GRAS status for the uses of a flavor ingredient in food does not provide regulatory authority to use the flavor ingredient in e-cigarettes in the US.
- E-cigarette manufacturers should not represent or suggest that the flavor ingredients used in their products are safe because they have FEMA GRAS status for use in food because such statements are false and misleading (Flavor and Extracts Manufacturing Association (FEMA) 2021).
In summary, some flavouring chemicals likely to be used in EC liquid may have been assessed as safe to ingest, but not to inhale.
The FEMA statement above is worth thinking about. Here is an association representing an industry which exists to promote and safeguard the interests of manufacturers of chemical flavours. Vaping would represent a massive additional source of demand for flavouring chemicals for the chemical companies in that industry. Yet here we have FEMA going out of its way to explicitly warn that no one should ever suggest that inhaling vapourised chemical flavours is safe as this would be false and misleading.
Flavours are a major factor in attracting people to vape. For example, 83% of New Zealand vapers named flavouring as a main reason they took up vaping (Gendall and Hoek 2021). We also know that flavours are a big factor that attract children and adolescents to vaping (Ranney 2019). Liquid nicotine manufacturers have paid close attention to these appeals. Here are a few examples of flavours that would be a big hit when announced at any five-year-old’s birthday party: Cherry Crush, Vivid Vanilla, Banana Split, Cotton Candy, Rocket Pop, Gummy Bears (Campaign for Tobacco-Free Kids 2014).
Vaping advocates argue that regulators should keep their hands off flavours because they are a major factor attracting smokers to try to keep vaping, which these advocates of course believe should be very much encouraged. As the then head of the Foundation for a Smoke-Free World, an agency entirely funded by the tobacco company Philip Morris International, tweeted on 21 February 2021, “E-cigarette flavor bans will drive more people back to smoking – InsideSources. Responsible regulators should take note. In their zeal to address youth vaping they may well undermine the health of millions of smokers seeking to switch. @US_FDA” (Yach 2019).
So apparently, those concerned to stem the dramatic rises in regular vaping by teens in several nations which have followed the opening the e-cigarette access floodgates should get their priorities right. They should always put the interests of adult vapers ahead of preventive efforts to reduce the uptake of vaping by children.
The US Food and Drug Administration (USFDA) in late August 2021 took a decidedly different view of the risk–benefit balance when it came to flavoured vapes. Announcing that it had issued marketing denial orders over 55,000 flavoured vaping products submitted by three manufacturers, it said the applications “lacked sufficient evidence that they have a benefit to adult smokers sufficient to overcome the public health threat posed by the well-documented, alarming levels of youth use of such products” (US Food and Drug Administration 2021a). By September 2021, 295 Marketing Denial Orders had been issued by the USFDA for flavoured NVPs which impacted an estimated 1,089,000 flavours (Tobacco Business 2021).
Jordt et al. using gas chromatography, mass spectrometry and nuclear magnetic resonance spectroscopy and observed that:
flavour aldehydes such as vanillin (vanilla flavor) and benzaldehyde (berry/fruit flavor) rapidly undergo chemical reactions with the E-liquid solvents PG and VG after mixing. The chemical adducts formed, named aldehyde PG/VG acetals, are carried over into the aerosol and are stable at physiological conditions.
Toxicological tests reveal that these compounds activate the sensory irritant receptors TRPV1 and TRPA1, involved in triggering cough, secretions and cardiovascular reflexes to irritant inhalation. The aldehyde acetals activate these receptors more robustly and potently than the parent aldehydes. Comparison of the cytotoxic effects of parent aldehydes and acetals in cultured bronchial epithelial cells demonstrate that acetals induce cell death at lower concentrations. Analysis of mitochondrial respiration and glycolysis reveal that flavor aldehyde acetals suppress mitochondrial oxygen consumption and ATP production.
These findings suggest that electronic cigarettes release unstable chemical mixtures containing a large variety of chemical products with unexpected toxicological properties (Jordt, Caceres et al. 2020).
In summary, the authors found that “flavourings combine with solvents in e-cigarettes to produce new toxic chemicals that irritate the airways, triggering reactions that can lead to breathing and heart and blood vessel problems”. The lead author commented, “This is the first demonstration that these new chemicals formed in e-liquids can damage and kill lung cells and probably do this by damaging their metabolism. Although, in some cases, more than 40% of flavour chemicals are converted into new chemicals in e-cigarettes, almost nothing was known about their toxicity until now” (European Lung Foundation 2020).
Despite such evidence, a 2021 review of 58 research reports on e-cigarette flavours and young people found “no included reports of adverse effects of flavours” in studies where the “quality of the evidence was very low”. The authors nonetheless found that the evidence “suggested that flavours are important for initiation and continuation of vaping. Qualitative evidence shows interest and enjoyment in flavours” (Notley, Gentry et al. 2021), which explains a great deal about why vaping interest groups defend flavours to the death.
In November 2020, Clive Bates gave evidence to the Australian Senate’s inquiry into vaping (Australian Senate 2020a):
Senator Urquhart: A lot of these flavourings are approved for ingestion in foods but not for inhalation into your lungs.
Mr Bates: You’re right. Many of them haven’t been evaluated for inhalation. They are generally recognised as safe as food additives and they’re added to these products to make them appealing. So you’re right. They don’t have —
Senator Urquhart: I don’t want to cut you off. I don’t want to do that at all, but I am pressing for time. I just want to try and get the justification for how it can be safe to inhale stuff that is not meant to be inhaled into your lungs …
Mr Bates: … With vaping, they’re not moving to a situation where they’re inhaling chemicals we know to be dangerous – where there are known dangers, the manufacturers tend not to put them in – but they’re moving to inhaling chemicals that at least at one level have been recognised as safe for ingestion. But you’re perfectly correct; most of the flavours have not been evaluated as safe for inhalation.
This is why the vaping industry and its facilitators have fought proposals for therapeutic regulation and instead want their products to bypass safety standards that they would try in vain to demonstrate.
Instead, they effectively argue that the public health and human rights imperatives to allow unimpeded access to vaping are so stratospherically important that e-cigarettes should be accorded exceptional status, allowing them to be exempted from any regulations that might prevent maximum uptake. This of course is an argument that has often been made by purveyors of quack cures for a wide range of deadly diseases, including cancer, HIV and COVID-19 (Dyer 2018, Australian Associated Press 2021). No sensible person believes that breathless claims and testimonies for these shonky and often dangerous treatments should raise them above regulatory scrutiny, but many evangelical vaping advocates believe NVPs are too important to be seriously regulated.
Without the choice of thousands of untested flavours, they argue that many vapers would abandon vaping, regardless of their conviction that these products are saving their lives. Yet people living with asthma who know that salbutamol is critical for control of asthma attacks don’t abandon their unflavoured puffers because they don’t taste the best.
How many puffs a day do vapers take?
Finally, there is also an important difference between inhaling flavoured nicotine and using an asthma puffer or attending a theatre performance once in a while when theatrical fog using propylene glycol (also found in EC vapour) might waft into the audience for a minute or two. People who use asthma puffers are advised that it is safe to use them 4–6 times a day maximum. Let’s contrast this with the number of times that the average vaper fills their lungs with propylene glycol, nicotine and flavouring chemicals, all vaporised from the liquid that is heated by the metal coil heated by the e-cigarette battery.
A 2020 study monitoring vaping found those who were exclusive vapers pulled this cocktail deep into their lungs from point-blank range on average 173 times a day – 63,188 times a year. Those who were dual users (i.e. who vaped but still smoked) basted their lungs 72 times a day with their e-cigarettes in addition to the smoke from their smoking (Yingst, Foulds et al. 2020). Another study found the average daily number of puffs taken was 200, with a range up to 611 (Martin, Clapp et al. 2016). A third study, where researchers observed vapers using their normal vaping equipment ad libitum (as often as they pleased) for 90 minutes, reported the median number of puffs taken over 90 mins was 71 (i.e. 0.78 puffs per minute or 47.3 per hour) (St Helen, Ross et al. 2016). If a person vaped for 12 hours a day at that rate, this would translate to 568 puffs across a 12-hour day or 207,462 times in a year.
We can contrast this with the number of puffs today’s average 12-cigarettes-a-day smoker inhales. One study observing puff frequency in those smoking in social settings recorded an average of 8.7 puffs per cigarette with an average 38.6-second gap between puffs (Chapman, Haddad et al. 1997). At 12 cigarettes a day, this would translate to 104 puffs per day or 38,106 per year. So vapers’ puffing compared to smoking occurs at an almost frantic rate, making a mockery of the bizarre denialism often seen in vaping chat rooms insisting that vaped nicotine is not addictive.
Evidence on the effectiveness of e-cigarettes in smoking cessation
On 6 July 2017 submissions closed on an Australian House of Representatives committee considering the regulation of e-cigarettes. The 332 submissions included many individuals’ personal stories explaining that e-cigarettes had succeeded in helping them quit when other methods had failed (House of Representatives Standing Committee on Health, Aged Care and Sport 2017). Many wrote passionately about having tried and failed with other ways of stopping smoking. Some made statements about their health rapidly improving. They wanted to spread their good news and encourage others to try to do what they had done. Many of these stories would have been very real: most of us have heard of someone who has quit through vaping.
It is certainly true that around the world there are many such cases. But just as we would never conclude that drink-driving was not risky after counting the number of people who drove after drinking and suffered or caused no harm, we should never conclude that any given method is an effective way to quit smoking by listening only to those who say they have benefitted from it.
Parliamentary inquiries into quackery such as homeopathy and naturopathy would doubtless see passionate submissions from former smokers about how these methods had helped them quit. But the public policy question is whether such strategies actually make smoking cessation more likely when studied under suitably controlled research conditions.
As I discussed in Chapter 2, we do not assess evidence on smoking cessation by only considering examples of success. There were no submissions to the House of Representatives committee from the smokers who had switched to vaping but failed or did not even attempt to quit, as there were no such submissions to yet another inquiry held by the Australian Senate in 2020 (Australian Senate 2020b). Yet in 2019, there were close to half a million such people in Australia who had started vaping but no longer did, almost double the number of current daily vapers (see Table 6.1).
The 2019 national data in Table 6.1 are sourced from the Australian Institute of Health and Welfare’s national household survey where the AIHW describes “current” vaping (in a footnote to Table 2.23) as including people who reported “using electronic cigarettes daily, weekly, monthly or less than monthly”. So that means “current vaping” in the last year includes people who might have had a puff or two at a party out of curiosity, 15-year-olds passing an e-cigarette around after school once or twice at the local skate ramp and those who bought vaping gear, tried it a few times and then put it in the drawer with other seemed-like-a-good-idea-at-the-time, five-day wonders.
Had I been swept up in such an AIHW sample a few years ago, the “current vaping” cohort also would have included me because I once had a pull on an e-cigarette to see what it was like. So are many of these 527,000 people any more meaningfully “current” vapers than I am a current Aston Martin driver (because I’ve driven one once), a current Chateau Laffite drinker (I shared one with friends once) or a current guest at Australian prime ministers’ houses (because I attended a fundraiser at one once)?
Table 6.1 Vaping status of Australian e-cigarette users (Source: Australian Institute of Health and Welfare 2020c).
| Vaping status | % of those who have ever vaped | Estimated number |
|---|---|---|
|
Daily |
9.4 |
222,000 |
|
At least weekly (but not daily) |
5.1 |
127,447 |
|
At least monthly (but not weekly) |
3.4 |
80,298 |
|
At least monthly |
17.9 |
422,744 |
|
Less than monthly |
4.4 |
103,915 |
|
“Current” vaping |
|
526,659 |
|
I used to use them, but no longer use |
18.1 |
427,468 |
|
I only tried them once or twice |
59.6 |
1,407,573 |
Vaping advocates pitch their most emotional appeals for policy change around profiles of heavy smokers who they say have often tried to quit and failed. This profile could only reasonably be applied to daily vapers, not those who smoke every day and vape very occasionally, nor those who are not nicotine dependent and neither smoke nor vape every day. So this means we are talking about some 222,000 Australians 14 years and over who are daily vapers in a population of some 25 million people. A substantial proportion of this group will be dual users who continue to vape and smoke and, importantly, have no plans to quit.
This is because it is very wrong to imply that all who are vaping today are former and current smokers who started vaping to quit smoking. The 2019 AIHW survey (at Table 2.32) reported that 51.2% of current e-cigarette users vaped to try and help them quit smoking. A recent paper from the ITC Four Country Survey (Australia, USA, UK, Canada) found that “among smokers who also vaped, 46% planned to quit smoking within six months, 30% planned to quit in the future, but beyond six months, with the remaining 24% reporting that they did not know or did not plan on quitting, suggesting low motivation to quit smoking among many of the concurrent [both smoking and vaping] users” (Gravely, Cummings et al. 2021). “Planning to quit” is also a very soft, rubbery measure, liable to be pregnant with social desirability response biases and often not full of much conviction.
So it is very clear that many dual users (who both vape and smoke) are not at all desperate or even interested in quitting smoking. We need to strongly oppose regulatory policy which puts the flavour-experimenting interests of vapers who don’t intend to quit ahead of policies that keep beguilingly flavoured vapes well out of the reach of children.
Recent reviews of the evidence on cessation
I’ll now summarise what we know from the best evidence available about how well NVP users go with quitting smoking. The following 17 reviews of the evidence and position statements by professional health associations published since 2017 have concluded that the evidence for e-cigarettes being effective for smoking cessation is inconclusive, insufficient, weak or inadequate:
- (2021) Wang et al: Meta-analysis of 55 observational studies: “As consumer products, in observational studies, e-cigarettes were not associated with increased smoking cessation in the adult population” (Wang, Bhadriraju et al. 2021).
- (2021) Zhang et al: “Evidence from 9 cohort studies showed that e-cigarette use was not associated with cessation” (Zhang, Bu et al. 2021).
- (2021) WHO: “To date, evidence on the use of ENDS [Electronic Nicotine Delivery Systems] as a cessation aid is inconclusive” (World Health Organization 2021).
- (2021) US Preventive Health Services Task Force: “The USPHSTF concludes that the current evidence is insufficient to assess the balance of benefits and harms of e-cigarettes for tobacco cessation in adults.” (Krist, Davidson et al. 2021).
- (2021) WHO Study Group on Tobacco Product Regulation (TobReg): “There is insufficient evidence that HTPs (heated tobacco products) aid a switch from smoking. Therefore, claims should not be made to that effect. Even if future evidence supported HTPs as effective switching aids (i.e. substituting one tobacco product for another), they should never be considered as treatment for smoking cessation, which includes quitting nicotine use” (WHO Study Group on Tobacco Product Regulation 2021).
- (2021) European Commission’s Scientific Committee on Health, Environment and Emerging Risks (SCHEER): “There is weak evidence for the support of electronic cigarettes’ effectiveness in helping smokers to quit while the evidence on smoking reduction is assessed as weak to moderate” (Scientific Committee on Health 2021).
- (2020) United States Surgeon General’s report on smoking cessation: “there is presently inadequate evidence to conclude that e-cigarettes, in general, increase smoking cessation” (United States Surgeon General 2020).
- (2020) Ireland’s Health Research Board: “there is no evidence of a difference in effect on incidences of smoking cessation. There is a low-level of certainty in these results due to low successful event rates and high rates lost to follow-up in all studies” (Quigley, Kennelly et al. 2020).
- (2020) Australian National University (preliminary report): “there is insufficient evidence that nicotine-delivering e-cigarettes are efficacious for smoking cessation, compared to no intervention, placebo existing nicotine-replacement therapy or other best-practice interventions” (Banks, Beckwith et al. 2020).
- (2020) Thoracic Society of Australia and New Zealand: “Smokers who enquire about using e‐cigarettes as a cessation aid should be provided with appropriate information about approved medication in conjunction with behavioural support (as these have the strongest evidence of efficacy to date). E‐cigarettes are not the first‐line treatment for smoking cessation” (McDonald, Jones et al. 2020).
- (2021) Grabovac and others (Effectiveness of Electronic Cigarettes in Smoking Cessation: a Systematic Review and Meta-Analysis): “nicotine-ECs may be more effective in smoking cessation when compared to placebo ECs or NRT. When compared to counselling alone, nicotine ECs are more effective short-term but its effectiveness appears to diminish with later follow-ups. Given the small number of studies, heterogeneous design and the overall moderate to low quality of evidence, it is not possible to offer clear recommendations” (Grabovac, Oberndorfer et al. 2021).
- (2020) Public Health England: “The data presented here suggests [sic] that vaping has not undermined the declines in adult smoking.” Note that they presented no evidence that vaping, endorsed and widely promoted by PHE, had accelerated the decline in smoking in the UK. This is to my knowledge the first time that PHE has taken such a lukewarm position on the impact of vaping on smoking rates (McNeill, Brose et al. 2020).
- (2019) European Respiratory Society: “There is not enough scientific evidence to support e-cigarettes as an aid to smoking cessation” (Bals, Boyd et al. 2019).
- (2018) US National Academies of Science, Engineering and Medicine – a “review of reviews”. “Conclusion 17-1. Overall, there is limited evidence that e-cigarettes may be effective aids to promote smoking cessation” (National Academies of Science, Engineering and Medicine 2018).
- (2018) European Public Health Association: “e-cigarettes may help some smokers quit but, for most, e-cigarettes depress quitting” (European Public Health Association 2018).
- (2018) CSIRO Australia: “While many smokers and former smokers state a preference for e-cigarettes as a smoking cessation method, the effectiveness of this method compared with other smoking cessation methods is not known” (Byrne, Brindal et al. 2018).
- (2017) El Dib et al.: A systematic review and meta-analysis of three RCTs and nine cohort studies concluded: “There is very limited evidence regarding the impact of [e-cigarettes] on tobacco smoking cessation, reduction or adverse effects: data from RCTs are of low certainty and observational studies of very low certainty. The limitations of the cohort studies led us to a rating of very low-certainty evidence from which no credible inferences can be drawn” (El Dib, Suzumura et al. 2017).
It remains true that, as summarised in the 2020 US Surgeon General’s report on smoking cessation, and cited as recently as October 2020 in an authoritative article by the heads of the US Centers for Disease Control, the Food and Drug Administration and the National Cancer Institute in the New England Journal of Medicine, “there is presently inadequate evidence to conclude that e-cigarettes, in general, increase smoking cessation” (Redfield, Hahn et al. 2020).
Randomised controlled trials (RCTs)
A 2021 Cochrane update of the evidence from three concluded randomised controlled trials on e-cigarettes in smoking cessation concluded that there was “moderate-certainty evidence, limited by imprecision, that quit rates were higher in people randomized to nicotine EC than in those randomized to nicotine replacement therapy (NRT) (risk ratio (RR) 1.69, 95% confidence interval (CI) 1.25 to 2.27; 3 studies, 1498 participants)” (Hartmann-Boyce, McRobbie et al. 2021).
In terms that the general public might better understand, the review stated, “For every 100 people using nicotine e-cigarettes to stop smoking, 10 might successfully stop, compared with only six of 100 people using nicotine-replacement therapy or nicotine-free e-cigarettes, or four of 100 people having no support or behavioural support only.” Or to put it another way, if we take 100 smokers participating in an RCT, 90 would still be smoking six months later if they used e-cigarettes, compared with 94 who used NRT, and 96 who just tried to quit alone or got some “behavioural support”.
Australian vaping advocates tried valiantly to spin this as e-cigarettes having been “proclaimed by the gold standard of RCT evaluation as being 70% more effective than NRT”, presumably taking the RR of 1.69 as being the most flattering angle that they could find.
But there can be few if any other drugs, used for any purpose, which have even come close to the dismal success rate of e-cigarettes or NRT in achieving their main outcome. If we went along to a doctor for a health problem and were told, “Here, take this. It has a 90% failure rate. But let’s both agree to call this successful,” we would understandably take the view that “success” when used in this context was not the way that it is used in any other treatment context, or indeed any context.
Importantly, as we saw in Chapter 2, results obtained from RCTs do not reflect those obtained in real-world use where “success” is often even much worse. RCTs exclude many people from high smoking prevalence population sub-groups (e.g. those with mental health problems, drug and alcohol problems); participants in RCTs are subject to a wide range of cohort retention strategies to prevent them dropping out of the trial – as happens commonly in real-world use; and participants are paid and given free quit-smoking medication (including e-cigarettes).
When considered together, all the above problems make the match with RCTs on smoking cessation a far cry from the way smokers use NRT and e-cigarettes in the real world. But this has not stopped wide-eyed commentaries about “effectiveness”, as if these artificially constructed trials bore any resemblance to the spread, patterns and conditions of use in communities.
Let’s look in more detail at one of the most recent RCTs.
In February 2019, Hajek and others published results in the New England Journal of Medicine of an RCT of nicotine replacement therapy (NRT n=446) versus use of a second-generation refillable e-cigarette device (n=438). Subjects were all self-selecting attendees at UK National Health Service stop-smoking services (Hajek, Phillips-Waller et al. 2019). Randomisation into the different arms of the RCT began after they had set a quit date. Astonishingly, dual users (the most common way that e-cigarettes are used) were excluded. So this was a study of smokers who were anything but a random sample of smokers from the UK smoking population.
The paper attracted considerable attention as it was a randomised study with an active control arm and used modern e-cigarette devices. Compared to previous RCTs which used earlier generation e-cigarettes, it had a substantially greater effect size with a relative risk of 1.75–1.84 (depending on adjustments and exclusion of certain subjects) for the primary outcome variable of continuous abstinence at 52 weeks. In media coverage, this effect was often rounded up to a doubling of smoking cessation compared to NRT.
Largely unreported in news coverage of this study was that ongoing use of e-cigarettes by 80% of subjects in the EC arm did not prevent relapse – the relative risk of relapse by 52 weeks in those who quit with EC rather than NRT was 1.27.
Significantly, all trial participants also received “weekly behavioural support for at least 4 weeks”, with the authors noting in their conclusion that “E-cigarettes were more effective for smoking cessation than nicotine-replacement therapy, when both products were accompanied by behavioral support” [my emphasis]. This support “involved weekly one-on-one sessions with local clinicians, who also monitored expired carbon monoxide levels for at least four weeks after the quit date”. Eighty-one percent of participants received four or five support sessions. So this was far from being a “brief advice” intervention situation.
However, in real-world use of either NRT or e-cigarettes for smoking cessation, only a tiny proportion of smokers ever receive such support. Important questions therefore arise about the relative contributions of NRT and NVPs, compared with that of the support which all trialists received. A study of a national English prospective cohort of 1,560 smokers found “the adjusted odds of remaining abstinent up to the time of the six-month follow-up survey were 2.58 times higher in users of prescription medication in combination with specialist behavioral support”. Notably though, the use of NRT bought over the counter was associated with a lower odds of abstinence (odds ratio, 0.68), compared with smokers not using NRT (Kotz, Brown et al. 2014). In other words, using NRT without behavioural support might be actually preventing some from quitting. It’s possible that the same might be true for e-cigarettes. But because all participants received behavioural support, we will never know.
Late in 2021, results of an Australian RCT were published (Morphett, Fraser et al. 2021). In a pragmatic trial that sought to assess quitting outcomes in as naturalistic conditions as possible (reflecting many of the concerns I raised in Chapter 2), smoking participants were randomised into three groups. One group was offered free first generation (cigalike), unflavoured ECs and/or NRT. At seven months’ follow-up a desultory 1.3% (8 of 619) assigned to that group self-reported that they were no longer smoking. Vaping advocates will shrug off this result, pointing out the irrelevancy in 2021 of a trial of first-generation, unflavoured cigalikes, which very few vapers use today. But an interesting question remains: why did a trial which was conducted in 2014–15, with 12 months’ follow-up, take until December 2021 to be published? It is difficult to imagine any circumstance where a trial showing positive results would have remained unpublished for such a time.
Cessation and dual use (vaping and smoking)
Before looking further at the evidence from longitudinal cohort studies of the effectiveness of NVPs in smoking cessation, it’s important to note that there is evidence of under-reporting of continuing smoking among vapers. Using biomarker data on the tobacco-specific nitrosamine NNK from those who provided it in the PATH study, Goniewicz and Smith estimated that one in six of those self-reporting as exclusive vapers were still smoking (Goniewicz, Smith et al. 2018). This major caveat should be kept in mind when reading summaries of the research on quitting to follow.
Unlike NRT, where persistent use is uncommon after six months (2.3% of NRT gum users, 0.9% for patch, with 0.4% persistent use of any NRT after 24 months) (Shiffman, Hughes et al. 2003), those who take up vaping can stay with it for years.
And importantly, a majority of those who vape also smoke (dual use). A stock tenet of vaping advocacy theology is that anyone who is a dual user should always be understood to be perpetually in the process of transitioning to completely quitting smoking. It doesn’t matter how long they have been vaping: if they are still smoking, they are still working hard on quitting smoking and should never be seen as a person who is smoking and vaping and not planning to stop either. Repeat often: dual users should always be counted as success stories in progress. If you follow a dual user down the track from when a cohort study first counts them as a dual user, at some future follow-up when they are interviewed, they are highly likely to have kicked smoking and now be an exclusive vaper, so the theology goes.
US PATH cohort study findings
Unfortunately for that argument, we have excellent longitudinal cohort data from the USA that shines bright warts-and-all-revealing light on its veracity. The US Population Assessment of Tobacco and Health (PATH) project (funded by the USFDA and the National Institutes of Health) has been collecting national cohort data on 46,000 Americans since 2013 (Hyland, Ambrose et al. 2017). These are the best data we have on real-world use of NVPs, and with PATH’s longitudinal design involving interviews with the same individuals every year, analyses from the data are peerless as a guide to the effectiveness of NVPs, unconstrained by the many limitations of RCTs that I discussed in Chapter 2.
I noted earlier that many who vape and keep smoking have little serious interest in quitting. With this being the case, analyses of quit rates among all who vape are bound to be heavily diluted by the inclusion of such vapers in the denominators of the studied population. Many dual users continue to smoke and vape at follow-ups because they were never interested in quitting. This has seen researchers report results for frequent vapers apart from those of all vapers, reasoning that infrequent vapers were probably far more likely to be smokers not trying to transition. A PATH report by Glasser and colleagues analysed three waves of PATH data from 2013 to 2016. Like other PATH studies, the odds of quitting when all vapers were included, were found to be insignificantly different to those smokers who didn’t vape. But “consistent and frequent e-cigarette use over time is associated with cigarette smoking cessation among adults” (Glasser, Vojjala et al. 2021). So it follows that frequent use of e-cigarettes being associated with higher quit rates should be seen as encouraging news, yes? Undoubtedly, except when we take a close look at the desultory numbers involved.
There were 5,894 participants using e-cigarettes at the beginning of the study. But only 78 (1%), were “consistent and frequent” users of e-cigarettes. For that 1% of users, quitting with e-cigarettes was more successful, but this was hardly a finding signalling that we are looking at results portending a major population-wide tsunami of quitting via vaping in the USA. If we take all who vape together, there’s no net story about way more quitting than when we compare smokers who don’t vape.
And another question we might ask here is about how many vapers who were trying to quit smoking also stopped using e-cigarettes by the 2016 follow-up? The Glasser paper does not provide that data. But Pierce and colleagues, analysing the same PATH data sets across the same years did look at this question (Pierce, Benmarhnia et al. 2020). Are you ready?
“None in the daily e-cigarette use group (n=56) and 45% of the no e-cigarette group (n=162) were abstinent from all tobacco (including e-cigarettes) for 12+ months at Wave 3.” Not one e-cigarette user who was using e-cigarettes to quit was able to quit both cigarette and e-cigarettes after three years. The heat generated from the excited rubbing of hands together in Big Tobacco boardrooms on learning this must have been formidable.
Table 6.2 Summary of e-cigarette transitions from Wave 1 to Wave 2 by cigarette smoking status (n=2932) derived from (Coleman, Rostron et al. 2019).
|
Positive outcome at Wave 2 n=524 (17.9%) |
Negative outcome at Wave 2 n=1116 (38%) |
Remained the same n=1291 (44%) |
|---|---|---|
| 143 dual users who quit EC and smoking | 886 dual users who relapsed to smoking exclusively | 902 dual users continuing as dual users |
| 104 dual users who became exclusive EC users | 109 exclusive EC users who progressed to smoking | 389 EC users continuing as exclusive EC users |
| 277 exclusive EC users who quit EC | 121 exclusive EC users who progressed to dual use |
Another PATH paper by Coleman and others reported on a 12-month follow-up (Wave 1 to Wave 2) of 2,932 vapers (Coleman, Rostron et al. 2019). Table 6.2 using data from the paper shows that for every person vaping at the Wave 1 assessment who benefitted across 12 months by quitting smoking and/or e-cigarettes, there were 2.1 who either relapsed or took up smoking having not been a smoker at baseline. The single most populous subgroup in the cohort were those who were dual users at wave 1 and remained dual users at Wave 2.
Ongoing dual use is not a beneficial, harm-reduction outcome from using e-cigarettes (I will look at the evidence for reducing smoking as compared with not smoking later in this chapter). So if we add these “stayed the same” dual users to those with negative outcomes in the left-hand column of the table, then for every positive outcome (left column), there were 3.85 negative outcomes in this cohort. Most disturbingly, in this adult cohort, nearly one in four of those who had never been established smokers took up smoking after first using e-cigarettes.
Another PATH paper (Dai and Leventhal 2019) found that in long-term quitters, relapse to smoking was 1.8%, 10.4%, 9.6% and 15% among never, prior, current occasional and current regular baseline e-cigarette users respectively. So regardless of how long people had vaped, relapse to smoking was between five and eight times higher than in those smokers who had quit but had never vaped. Big Tobacco could only be delighted by the 10% lapsing of long-term ex-smokers and 15% of vapers back to smoking. These were people they probably considered they had lost forever.
Still another PATH longitudinal paper (McMillen, Klein et al. 2019) reported that former smokers who had quit a long time ago but who vaped were far more likely than those who had never vaped to relapse back to smoking and that vapers were far more likely than those who had never vaped to have transitioned from being never smokers to smokers:
Distant former combustible cigarette smokers who reported e-cigarette past 30-day use (9.3%) and ever use (6.7%) were significantly more likely than those who had never used e-cigarettes (1.3%) to have relapsed to current combustible cigarette smoking at follow-up (P <.001). Never smokers who reported e-cigarette past 30-day use (25.6%) and ever use (13.9%) were significantly more likely than those who had never used e-cigarettes (2.1%) to have initiated combustible cigarette smoking (P < .001). Adults who reported past 30-day e-cigarette use (7.0%) and ever e-cigarette use (1.7%) were more likely than those who had never used e-cigarettes (0.3%) to have transitioned from never smokers to current combustible cigarette smokers (P <.001). E-cigarette use predicted combustible cigarette smoking in multivariable analyses controlling for covariates.
Across 12 months follow-up, PATH data from 1,082 dual users of tobacco cigarettes and e-cigarettes, found 88.5% of dual users continued smoking, although the odds of being smoke-free at follow-up were higher among dual users who vaped every day (Miller, Smith et al. 2020).
As I’ve emphasised, not all vapers are trying to quit, so it is important to focus on long-term abstinence among those who tried to quit with and without use of e-cigarettes as a cessation aid. Another PATH paper looked at 2,535 adult smokers in 2014-2015 (baseline assessment), who, in 2015–16 reported a past-year attempt to quit and the cessation aids used, and then reported smoking status in 2016–17 where continuous abstinence from smoking for 12 months or more was the key outcome (Chen, Pierce et al. 2020). They found that among smokers using e-cigarettes to quit, 12.9% succeeded in long-term abstinence. But this was no different to the results seen in those trying to quit who did not use e-cigarettes. And some two-thirds of e-cigarette users who quit smoking kept vaping.
Again using PATH data from Waves 1–3 (2013–16), Osibogun et al (2020) examined transitions of adult dual users. Among 1,870 adult dual users at Wave 1, after two years, 55.2% had relapsed to smoking, 25.7% remained dual users (so 80.9% were still smoking) 7% were exclusively vaping and 12.1% reported no past-month smoking or vaping. They found that greater nicotine dependence was associated with decreased relative risk of no past-month tobacco use (Osibogun et al 2020).
In late 2021, Kasza et al. reported from PATH data from waves 2–5 (October 2014 to November 2019) that daily vapers who expressed no interest in quitting at Wave 1 were more likely to quit cigarette smoking than those who did not vape, while non-daily vapers were less likely to quit (although this effect was not statistically significant). The major limitation of this paper was the very small number of quitters – just three among the non-daily vaping group and 17 among those who vaped daily. Across the years of the study there were 2,489 data records from 1,600 individuals, so by only focusing on those smokers who indicated no intent to quit at the beginning of the wave series studied, and considering attrition from the cohort, this left a very small group with the outcomes described. A footnote to a table warned “Estimate should be interpreted with caution because it has low statistical precision” (Kasza et al. 2021).
A 2020 paper from the ITC Four Country Survey (Australia, USA, UK, Canada) found that after 18 months:
smokers with established concurrent use [smoking and vaping] were not more likely to discontinue smoking compared to those not vaping … it is clear that the rates of transitioning away from smoking remain unacceptably low, and perhaps current vaping tools at best bring the likelihood of quitting up to comparable levels of less dependent smokers. The findings of our international study are consistent with the findings of the US PATH transition studies, and other observational studies, in that most smokers remain in a persistent state of cigarette use across time, particularly the daily smokers [my emphases] (Gravely, Meng et al. 2020).
Big Tobacco, now with major investments in NVPs, would have had all its fingers crossed in the hope that dual use would be as common as it is. And if they are wise investors, they would be also very confident that the net effect of vaping proliferation throughout the population will be to keep far more people in smoking than are tipped out of it, and that it will provide high adoption of nicotine-addiction training wheels to many children and adolescents who have never used any form of nicotine and probably never would have done.
Is vaping the primary cause of falls in smoking prevalence in nations where vaping is prevalent?
There are many factors which can combine to cause changes in smoking prevalence over time. Vaping advocates argue that nations with widespread vaping are seeing their falls in smoking prevalence accelerate mostly because of vaping.
Figure 6.3 is constructed from Smoking in England data (West, Kale et al. 2021) and suggests that the role of e-cigarettes in accelerating the downward trend in smoking in England could only be modest. The dramatic upsurge in smokers using e-cigarettes in quit attempts commenced in late 2012. Use has more or less plateaued since mid-2013 and does not appear to have had any marked association with the downward slope of the historically declining smoking prevalence rate.
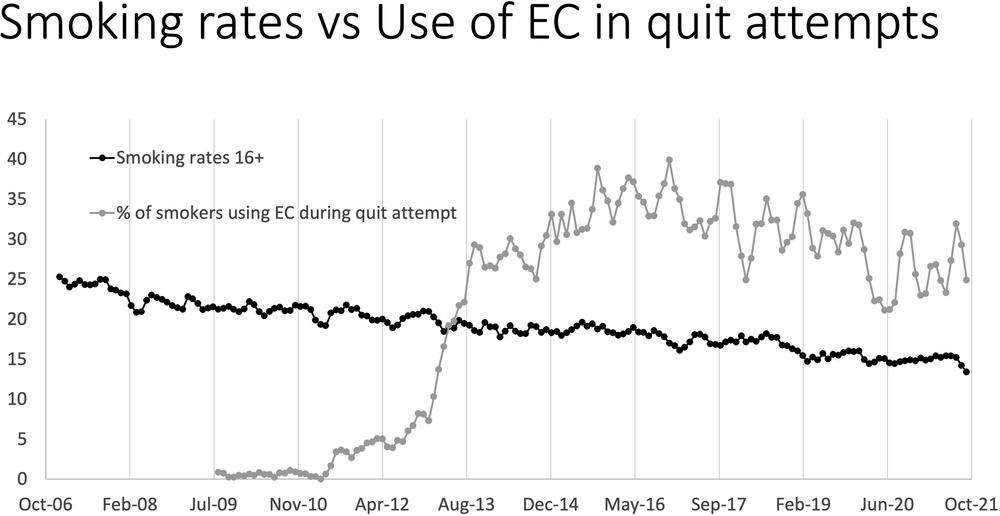
Figure 6.3 English smoking prevalence and quit attempts using e-cigarettes (Source: Data extracted from Smoking in England website.) Note: From April 2020, data were collected by phone and from people 18 years and over. Before then, data were collected by household visits from people 16 years and over.
However, if we look at the data on smoking prevalence and changes in tobacco affordability in the UK, we can see a rather different picture (Figure 6.4) (National Health Service Digital 2020). Smoking prevalence was falling well before vaping commenced and there is a close relationship between the decline in the affordability of tobacco and the fall in smoking prevalence. Cigarettes were 27% less affordable in the UK than they were in 2009. Vaping grew rapidly from around 2011 in the UK and did not alter the relationship between smoking prevalence and tobacco affordability.
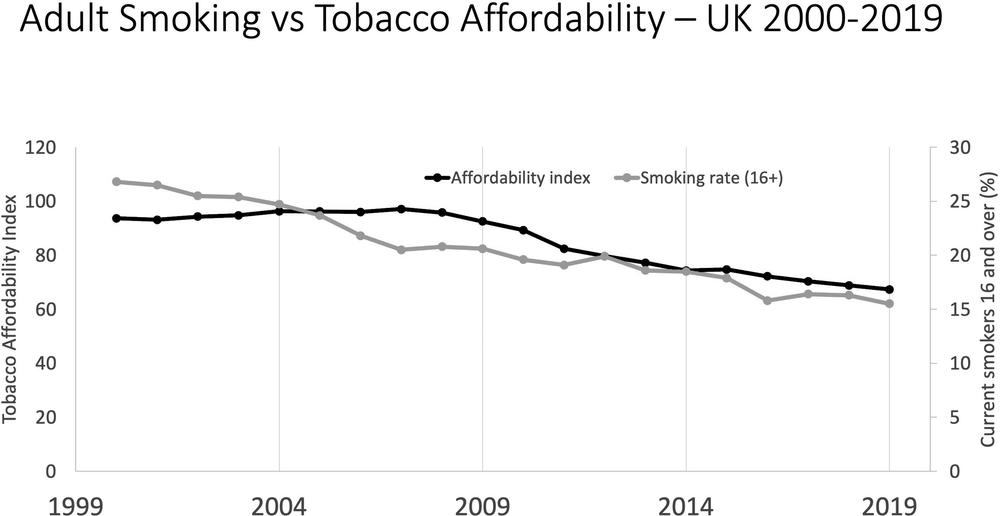
Figure 6.4 Changes in smoking prevalence in persons aged 15 and over and tobacco price index relative to retail price index (all items) 2000–19, UK. Source: Statistics on Smoking, England 2020; Smoking prevalence in the UK and the impact of data collection changes: 2020.
Researchers from the Smoking in England project published a step-by-step estimation of the number of English smokers whose smoking cessation in 2014 could be attributed to e-cigarettes (West, Shahab et al. 2016). They took into account factors like an estimated 70% relapse back to smoking and the fact that e-cigarettes displace success rates that would have occurred via other methods (which fewer people use with the rise of e-cigarettes).
The group estimated that 16,000 smokers quit permanently in a population of 8.46 million adult smokers. That’s about 0.19% shaved off England’s smoking population in one year by e-cigarettes – just one in 529 smokers in a year quitting permanently.
For perspective, in Australia where the prevalence of regular vaping in the same data period examined by the above report was very marginal (only 1.5% of Australia’s daily smokers and 0.8% of ex-smokers used e-cigarettes daily), smoking prevalence in those aged 14+ had declined over the 10 years between 2007 and 2016 (from 19.4% to 14.9%), an average of 0.45% a year. This decline reflected both smokers quitting and dying, and reductions in uptake.
Smoking prevalence has indeed fallen rapidly in England in recent years while e-cigarette use has increased. But it is simplistic to assume this is the only explanation needed. The trajectories for smoking prevalence and quit attempts differ from that for prevalence of use of e-cigarettes.
In fact, the reduction has occurred concurrently with a comprehensive program to reduce smoking. During that time there had been a spectacular decline in tobacco affordability, with cigarettes being 27% less affordable in 2016 than in 2006 (NHS Digital 2017) (see Figure 6.4).
Schooled by English experts
The Australian Senate Select Committee on Tobacco Harm Reduction’s report was published in 2020 (Australian Senate 2020b). I was lead author on a submission to the Senate inquiry along with Mike Daube from Curtin University and Matthew Peters, a professor of respiratory medicine (Chapman, Daube et al. 2020). Four English tobacco control experts, Ann McNeill (McNeill 2020) and Jamie Brown, Lion Shahab and Robert West (Brown, Shahab et al. 2020) read our evidence and wrote to the committee, seeking to advise them of our errors in understanding the impact of vaping on declining smoking prevalence in England. We were invited to reply. The exchanges are very relevant to this section of the chapter.
Response to letters from Professors Brown, Shahab and West, and Professor McNeill
Professors Brown, Shahab and West’s brief letter entitled Impact of e-cigarettes on smoking in England (Brown, Shahab et al. 2020) provides different conclusions from the data on the impact of e-cigarettes on smoking prevalence in England. They claim these conclusions as “the correct analyses”. We would, however, note that:
In their 2016 BMJ paper (cited in their letter) they wrote:
With quit attempts at 32.5% of eight million smokers (2.6 million) in 2015, and prevalence of e-cigarette use in quit attempts at 36% in that year, this equates to 54,288 additional short to medium term quitters in 2015 compared with no use of e-cigarettes in quit attempts. We would expect up to two thirds of these individuals to relapse at some point in the future, so we would estimate that e-cigarettes may have contributed about 18,000 additional long term ex-smokers in 2015. This figure is similar to that estimated indirectly using the estimated effect size of e-cigarettes and the numbers using them. Although these numbers are relatively small, they are broadly similar to previous estimates, and are clinically significant because of the huge health gains from stopping smoking. A 40 year old smoker who quits permanently can expect to gain nine life years compared with a continuing smoker. This number of additional quitters is unlikely to produce a detectable effect on smoking prevalence in the short term, but might be picked up over a period of several years [our emphases in italics] (Beard, West et al. 2016).
In their paper in Addiction, first published in 2019, they wrote:
845,152 smokers used e-cigarettes in quit attempts; this equates to 50,700 … additional past-year smokers who report that they are no longer smoking as a consequence of e-cigarette use in a quit attempt in 2017. This is broadly similar to the estimate which we reported for 2015 (Beard, West et al. 2020).
We note that in their Addiction paper, the authors did not discount that figure by two-thirds relapsing in the future, as they did in their BMJ paper. If we apply that discount to the 845,152 smokers who used e-cigarettes in a quit attempt (50,700 who were not smoking in 2017 x 0.33) we get 16,731 (2%) ... who, by the authors’ 2015 assumptions, would have quit in the long-term. (Expressed differently, 98% of smokers using e-cigarettes in quit attempts in England in a year are estimated to not quit in the long-term). This is a proportion very close to the quit rate (4%) for quit attempters allocated to no quitting support arms in the recent Cochrane trials update (Hartmann-Boyce, McRobbie et al. 2021).
So 16,731 of 7 million English smokers were additional long-term quitters in one year because of e-cigarettes: 1 in 418 of all English smokers. We heartily concur with Professors Brown, Shahab and West in their BMJ paper that “This number of additional quitters is unlikely to produce a detectable effect on smoking prevalence in the short term”. The number span 16,000–18,000 is not well expressed as “tens of thousands a year” as they wrote in the preface to their submission, so we remain curious about why they believe our interpretation of their data is incorrect.
Brown et al.’s BMJ paper states that there were 8 million smokers in England in 2015 and their Addiction paper says this number had fallen to 7 million in 2017 (a fall of approximately 12.5% or 6.25% per annum). If we assume there were three full years encompassed in the 2015–17 period, there were three years of approximately 17,000 estimated additional long-term quitters between 2015 and 2017, then some 51,000 (5.1%) of the extra 1 million who were not smoking in 2017 might be attributable to e-cigarette use. The other 949,000 fewer smokers would be attributable to deaths of smokers, cessation by smokers other than via e-cigarettes, and increasing numbers of never smokers thanks to prevention policies and programs.
Recent US longitudinal data from the PATH cohort study across five years 2013–17 (Brouwer, Jeon et al. 2020) found:
Cigarette use was persistent, with 89.7% (95% CI 89.1% to 90.3%) of exclusive cigarette users and 86.1% (95% CI 84.4% to 87.9%) of dual users remaining cigarette users (either exclusive or dual) after any one year
and
Among all W1 (Wave 1 or baseline) daily smokers, there were no differences in discontinued smoking between daily smokers who vaped (concurrent users) and exclusive daily smokers.
A preliminary report of a Swiss study of over 5,000 young men (Gmel, Wicki et al. 2020) found no cessation effects and that non-current smokers (never- and ex-) and smokers at baseline were more likely to be smokers four years later if they subsequently had started vaping. The authors concluded that:
Some smokers may have benefitted from using ECs, but they were few. At the general population level, ECs are not predominantly used in a way which might optimise reducing or ceasing smoking. Therefore, the public health effect on the general population of using ECs may be questionable, as may policy measures to facilitate EC use.
The 2020 Addiction paper showed that the proportion of smokers in England making quit attempts fell from almost 40% in 2013 to about 34% in 2017 (Beard, West et al. 2020). The definitions of quit attempts differ somewhat between the surveys used in different countries and quit rates will fall after periods when large numbers of smokers have already successfully quit (for instance, immediately following large tax increases). Nevertheless, in contrast to the 29% of smokers in England who made a quit attempt in 2019 (West, Kale et al. 2021) – the proportion of current smokers who report having attempted to quit in the previous 12 months in Australia – a country with much lower rates of use of e-cigarettes – was about 50% in 2007 and 2013 and was still 51% in 2019 (Australian Institute of Health and Welfare 2020d).
If the proportion of smokers trying to quit in England was approximately 50% rather than approximately 30%, an additional 1.4 million smokers would be making quit attempts each year, with an additional 56,000 likely to succeed even assuming no additional cessation support. The challenge for tobacco control in both nations is to simultaneously increase both the numerator of quit successes and the denominator of quit attempts.
All major companies in the global tobacco industry are now promoting putative harm-reduced products, while continuing to aggressively promote cigarettes. It is clearly in the industry’s interests to sell as much of both types of product as possible. If e-cigarettes put quitting in a prolonged holding pattern for many smokers and relapse to smoking is widespread, vaping may be holding many in smoking who might otherwise have quit.
Further data
Since we wrote that response, further salient information has come to hand from the UK Office for National Statistics data on the percentage of current smokers who have never vaped (Office for National Statistics 2020b). If widespread vaping was driving large-scale smoking cessation, it would follow that the proportion of current smokers who have never vaped would rise with time. Vapers who progressed to being ex-smokers would leave the pool of continuing smokers and persistent smoking would become concentrated in those who had stubbornly never vaped. Tables 6.3 and 6.4 show the data on the proportion of current UK smokers who have never vaped for the years 2015–19 – a period of heavy e-cigarette promotion.
However, these data and the trend within them could also be explained, or contributed to, by vaping leading to smoking. So it is important that we look at them the other way. If vaping were effective at a population level, the proportion of ex-smokers who had never been vapers should be declining. The ex-smoker pool should be enriched by current or past vapers who have recently quit and older ex-smokers who quit before the advent of vaping die off. Again, data on the proportion of ex-smokers who have never vaped is inconvenient to a narrative about vaping driving smoking cessation.
Table 6.3 Proportion of current UK smokers who have never vaped, 2015–19. Source: Office for National Statistics 2020b.
| Year | % who have never vaped |
|---|---|
| 2015 | 35.8% |
| 2016 | 35.4% |
| 2017 | 34.1% |
| 2018 | 33.7% |
| 2019 | 32.3% |
Table 6.4 Proportion of UK ex-smokers who have never vaped, 2015-19. Source: Office for National Statistics 2020b.
| Year | % who have never vaped |
|---|---|
| 2015 | 83.0% |
| 2016 | 77.6% |
| 2017 | 77.0% |
| 2018 | 76.9% |
| 2019 | 76.9% |
With England seeing major declines in the use of varenicline (−69.2% from peak in 2010) bupropion (−92.6% from 2001 peak) and NRT (−81.7% since the 2005 peak) (Statista 2021c, Statista 2021b, Statista 2021a) while vaping soared, it is likely that some of those who quit via vaping would have been smokers who might otherwise have quit using those methods. This positive figure – however large it actually is when the additional cessation forgone from these large reductions in use of other medications is netted out – needs to be contextualised against concerns that e-cigarettes may be holding many smokers in smoking who might otherwise have quit. As we have seen, there is considerable evidence that this is occurring.
Response to Professor McNeill’s letter titled “Additional Comment to the Australian Select Committee on Tobacco Harm Reduction”
Referring to our submission, where we wrote, “Relapse to smoking is very prevalent (A UK 15-month follow‐up of vapers (Brose, Bowen et al. 2019) found that overall 39.6% had relapsed to smoking, with those using tank systems faring worst (45.6%))”, Professor McNeill claims that this is misleading in a number of ways. She wrote:
Rather than go into the details, I copy here the conclusions of the study (Brose, Bowen et al. 2019), but would be happy to provide further information if required: “In a group of ex‐smokers who had stopped smoking for at least 2 months, relapse to smoking during a 15‐month follow‐up period was likely to be more common among those who at baseline vaped infrequently or used less advanced devices”.
As an author on the Brose et al. paper, McNeill would know that daily vapers in the study had almost exactly the same risk of relapse back to smoking as those who had never vaped (34.5% vs 35.9%). The clear messages from that paper are that vaping does not prevent relapse and that even daily vaping is barely different from not vaping in preventing relapse.
McNeill was also an author on a recent analysis of ITC Four Country Survey data which concluded not only that “Among all W1 (baseline) daily smokers, there were no differences in discontinued smoking between daily smokers who vaped (concurrent users) and exclusive daily smokers” but that “Most ex-smokers remained abstinent from smoking, and there was no difference in relapse back to smoking between those who vaped and those who did not” (Gravely, Cummings et al. 2021).
The great English success story of vaping?
Finally, drawing on recent data from the Smoking in England database from 18 November 2021 (West, Kale et al. 2021), my colleague Matthew Peters has described what he calls the “non-sensagon” – nine facets to the supposedly Great English Success Story of Vaping and Smoking:
- EC use has remained relatively stable since 2013 and the decline in smoking prevalence has plateaued since 2019.
- The proportion of 18–24-year-olds who have ever smoked rose from 24% in 2019 to 33% in 2020 and 34% in 2021.
- Cigarette smoking prevalence in 18–21-year-olds is up from 16.7% to 19.9% between 2019 and 2021.
- EC use among recent ex-smokers has declined from a peak in 2016.
- EC use for quitting has declined from a peak in 2016.
- Half of EC users are current smokers (dual users).
- Twenty percent of EC users are long-term ex-smokers (not active quitters).
- The most common quit strategy is unassisted (ECs are the most common quitting aid).
- Only 14% of vapers are using ECs for intended harm reduction.
New Zealand’s dramatic decline in adult smoking and rise in vaping
Just as the writing of this book was nearing completion, data was released in New Zealand on smoking and vaping for 2020–21. An excellent summary and commentary was published on the Public Health Expert blog (Edwards, Ball et al. 2021). Daily smoking prevalence in 2020–21 was 9.4% and current (at least monthly) smoking prevalence was 10.9% with the authors noting, “There was a steady, though unspectacular, decline in current and daily smoking prevalence of about 0.6% per year in absolute terms from 2011/12 to 2019/20. However, from 2019/20 to 2020/21, daily smoking prevalence fell by 2.5% and current smoking prevalence by 2.8%.” This fall was unprecedented.
Use of ECs was first assessed in 2015/16; since then, the prevalence of current and daily EC use has steadily increased. The increase in EC use was much greater in 2020/21: current EC use grew from 5.3% in 2019/20 to 8.2% in 2020/21 and daily EC use from 3.5% to 6.2% over the same period. The increase in daily and current EC use between 2019/20 and 2020/21 occurred concurrently with the large reduction observed in smoking prevalence [Figure 6.5], whereas the more gradual increase in EC use between 2015/16 and 2019/20 was not associated with a substantial change in the rate of decline in smoking prevalence.
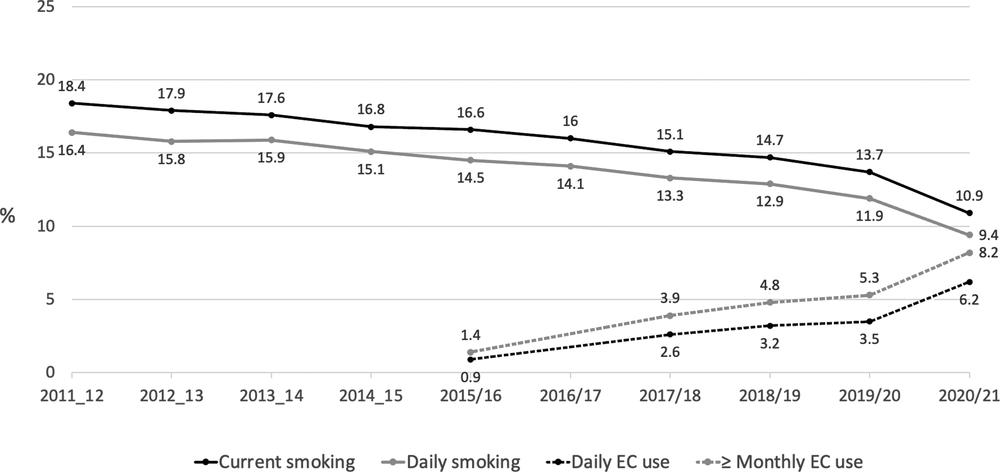
Figure 6.5 Trends in current (≥monthly) and daily smoking and e-cigarette use (NZHS 2011–12 to 2020–21) (Source: Edwards, Ball et al. 2021).
In their discussion, the blog authors emphasised that “caution is required when interpreting survey data and extrapolating trends from a single survey year”. They also explored several possible explanations for this fall, other than the rise in vaping which occurred most in younger adults in whom smoking also fell the most. These were: the chance that a random variation had occurred; that COVID-19 had caused people to quit out of generalised heightened concerns for health; and that other tobacco control policies were responsible. They found each of these unlikely to be as plausible as the role of vaping.
New Zealand then, presents today as a nation where the case for vaping reducing smoking through a quitting effect seems very plausible. However, as I discussed earlier in the chapter, there is important evidence that both vaping and smoking are also rising in school-aged children in New Zealand, concerning developments which no one but those profiting from this would applaud. In Chapter 8, I’ll discuss how vaping regulation policy might best ensure that smokers believing they might quit with NVPs can get access while children and those simply wanting to vape with little interest in quitting would find it harder.
Does vaping reduce smoking frequency (number of cigarettes smoked)?
Advocates for e-cigarettes also point to reduced smoking as a positive outcome from vaping. They emphasise that at the times when people are vaping they are not smoking as they otherwise would be likely to be doing. So across a day, month and year, vapers who still smoke are likely to smoke fewer cigarettes than if they did not vape. Obviously this is no-brainer evidence of harm reduction, they insist.
An early paper from the US national PATH cohort (Berry, Reynolds et al. 2019) found that daily e-cigarette smokers had 5.7 times the odds of reducing their average daily cigarette use by at least 50% compared with smokers in the cohort who did not vape. Daily vapers were also 7.9 times more likely than non-vapers to have stopped all smoking for at least 30 days. Given that many smokers take up vaping to try to quit or cut down their smoking, this almost certainly means that taking up vaping is a marker of attempting to quit. It was therefore quite predictable when comparing smokers not vaping with those who did, that a higher proportion would quit for at least a short time in the cohort who were vaping because vaping was a marker of trying to quit. Many smokers in the cohort who were not vaping were not even trying to quit. Across the time the longitudinal study was conducted, vaping was the most popular assisted method of trying to quit.
So what does the evidence say about whether reducing smoking, as opposed to quitting smoking altogether, actually reduces harm? While there is strong evidence for a causal association between disease and early uptake, amount smoked, and duration of smoking, the evidence on “reverse engineering” harm by continuing to smoke while cutting back is far from strong. We have good evidence from several large cohort studies conducted in Norway, South Korea, Scotland and the USA where smokers were followed up for several years and the health outcomes of those who reduced smoking over time compared with those who did not reduce.
A 2007 systematic review examining the health effects of reducing smoking by more than half found only “small health benefit” (Pisinger and Godtfredsen 2007). Since then, five cohorts (Tverdal and Bjartveit 2006, Song, Sung et al. 2008, Hart, Gruer et al. 2013, Inoue-Choi, Christensen et al. 2020) with a combined total of 1,011,120 people followed for up to 25 years have reported findings such as “no evidence that smokers who cut down their daily cigarette consumption by >50% reduce their risk of premature death significantly” (Tverdal and Bjartveit 2006). One of the largest, from South Korea (Song, Sung et al. 2008) found no association between smoking reduction and all cancer risk but a significant decrease in risk of lung cancer, but with the size of risk reduction “disproportionately smaller than expected”. A USA cohort with 505,500 people followed for different lengths of time between 1992 and 2011 concluded, “Although reducing smoking from daily to nondaily was associated with decreased mortality risk, cessation was associated with far greater benefit. Lifelong nondaily smokers have higher mortality risks than never smokers, even among those smoking 6 to 10 cigarettes per month. Thus, all smokers should quit, regardless of how infrequently they smoke” (Inoue-Choi, Christensen et al. 2020).
An important 2018 paper considered the surge in e-cigarette use in England and whether this was reducing the number of cigarettes being smoked at the population level across the country (Beard, Brown et al. 2018). The authors concluded:
No statistically significant associations were found between changes in use of e-cigarettes while smoking and daily cigarette consumption. Neither did we find clear evidence for an association between e-cigarette use specifically for smoking reduction and temporary abstinence, respectively, and changes in daily cigarette consumption. If use of e-cigarettes and licensed NRT while smoking acted to reduce cigarette consumption in England between 2006 and 2016, the effect was likely very small at a population level.
Data from 2019 from the UK government’s annual Opinions and Lifestyle Survey also show that the average number of cigarettes smoked daily by smokers who vape (8 a day) is almost identical to that by smokers who have never vaped (8.1 a day) (Office for National Statistics 2021).
These data echo comments by Robert West, former editor-in-chief of Addiction, on BBC Radio 4 in February 2016. At 7 min. 44 sec. West says, “Now, that raises an interesting question. If [e-cigarettes] were a game changer, if they were going to have the massive effect on, you know, everyone switching to e-cigarettes and stopping smoking, we might have expected to see a bigger effect than we’ve seen so far, which has actually been relatively small.” At 10 min. 40 sec., he continues, “We know that most people who use e-cigarettes are continuing to smoke and when you ask them they tell you that they are mostly doing that to cut down the amount they smoke. But we also know that they are smoking, it’s not really that much more different from what they would have done since they started using e-cigarettes” (Porter 2016).